Micro-Invasive Glaucoma Surgery (MIGS) has prompted a shift in the glaucoma treatment paradigm, enabling earlier surgical intervention for patients with mild-to-moderate disease. MIGS offers a safe and effective surgical solution that bridges the gap between medical management and invasive surgery.
In this article, we describe the latest innovation in MIGS technology, the iStent inject (Glaukos), which addresses glaucoma treatment at the time of cataract surgery, and we offer insights into effective co-management of patients who have received it.
Prevalence and Need
The largest percentage of patients with glaucoma (77%) have mild-to-moderate disease1 and is the population commonly seen by optometrists. Several factors are driving the move toward earlier glaucoma surgical intervention for these patients. IOP is the only modifiable risk factor of glaucoma, yet IOP fluctuation has been associated with poor medication compliance or nonadherence to prescribed regimens.2 Lowering IOP while eliminating variability may be an optimal surgical glaucoma treatment goal. In addition, 60% of patients who use topical IOP-lowering medications report symptoms of ocular surface disease.3 A surgical procedure that offers the potential of reducing medications may yield an improvement of ocular surface health.
The iStent inject Opportunity
Approximately one in five cataract patients are also using at least one IOP-lowering medication for glaucoma.4 With a safety profile similar to that of cataract surgery, the iStent inject is designed to treat patients with primary open-angle glaucoma, or POAG, who are undergoing cataract extraction. The iStent inject is clinically proven to significantly reduce IOP, and it may reduce reliance on IOP-lowering medications at the discretion of an eye care professional. Because the iStent inject is a one-time opportunity, it is important for optometrists to start the conversation with patients about their glaucoma treatment options, and, of course, work with a surgeon who performs these procedures.
About the iStent inject
Glaukos technology has been proven safe and effective worldwide with stents being implanted in more than 500,000 eyes in the last 10+ years. The next-generation design, the iStent inject, was approved by the Food and Drug Administration in 2018.
Like the iStent, the iStent inject bypasses the trabecular meshwork to gain access to Schlemm canal. It is the only MIGS device to deliver two multidirectional stents designed to restore natural outflow by accessing multiple collector channels. The iStent inject has a central inlet and four side flow outlets to optimize flow and collector channel access without relying on extreme dilation (Figure 1).
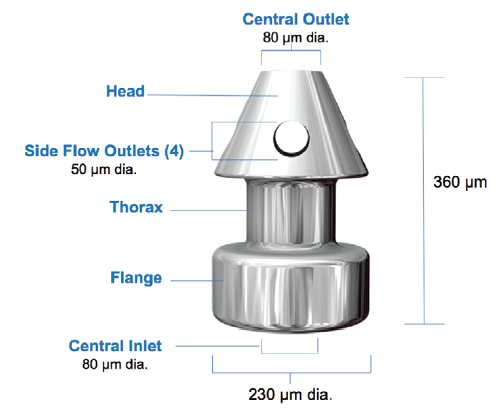
Figure 1. iStent inject design.
The surgical procedure for implanting the iStent inject is straightforward, astigmatically neutral, and minimally traumatic to the eye. Measuring at about one third of a millimeter in length, it is truly “micro” in scale and designed to be no larger than necessary to optimize natural aqueous fluid dynamics.
When implanting the iStent inject, the surgeon places the two multidirectional stents 2 to 3 clock-hours apart. Together, they deliver access to multiple collector channels and arcs of flow that can span 5 to 6 clock-hours. The iStent inject may also re-establish flow in previously dormant outflow channels.5,6
While surgeons appreciate the elegance of implanting the iStent inject, eye care professionals who comanage these patients report postoperative care and follow-up management similar to their experience with the original iStent and to that of cataract surgery.
Postoperative Care
Following a cataract surgery that includes the iStent inject, the comanaging optometrist usually supervises the patient’s use of an antibiotic and tapering of a steroid, manages topical IOP-lowering medications based on postoperative IOP, and integrates the patient back into his or her practice to provide ongoing glaucoma care.
Postoperative management of IOP-lowering medications for iStent inject patients is similar to the approach used for a typical cataract patient. Some practitioners stop IOP-lowering medications at the time of surgery, while others wait a couple of weeks after the surgery. Typically, this decision depends on the severity of the glaucoma. If a patient with mild glaucoma is responding well after the iStent inject procedure, the practitioner may stop the medication sooner. A patient who has moderate disease and some visual field loss may continue using the medication for a month or longer until the IOP is well controlled.
The iStent inject has an excellent and predictable overall safety profile similar to cataract surgery alone (Figure 2). Often, if an optometrist is comfortable comanaging patients who’ve had cataract surgery they are also comfortable comanaging patients who’ve had an iStent inject procedure.
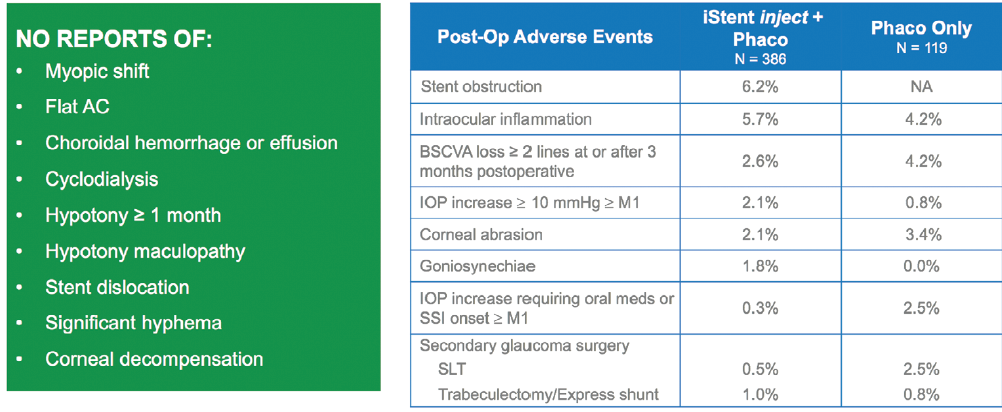
Figure 2. iStent inject pivotal trial.7
Pivotal Trial and Independent Studies
In the prospective, multicenter iStent inject pivotal trial, 505 eyes were randomly assigned to cataract surgery alone or cataract surgery plus iStent inject.7
At 24 months, investigators found the iStent inject outperformed cataract surgery alone, with 75.8% of eyes achieving a 20% or more reduction in unmedicated diurnal IOP (DIOP) (Figure 3). At 23 months, 84% of iStent inject subjects that were responders were medication-free. This demonstrates that the iStent inject has the ability to not only lower IOP but also can reduce patients’ reliance on IOP-lowering medications at the discretion of the physician.
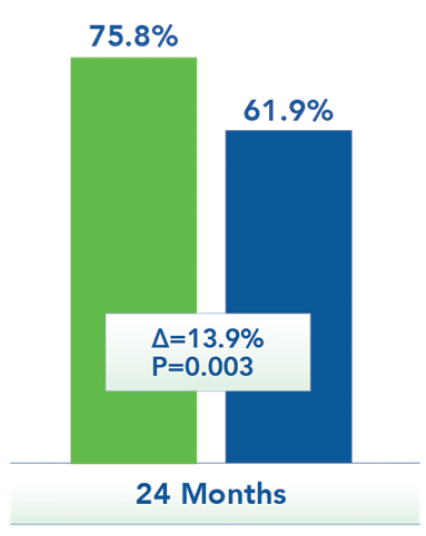
Figure 3. Percentage of eyes achieving ≥20% reduction in unmedicated DIOP.7
Figure 4 shows data from a consecutive case series of iStent inject patients collected by an individual surgeon in an independent study demonstrating durability over 3 years. Preoperative IOP was 22.6 ± 6.2 mm Hg and at 3 years was 14.3 ± 1.7 mm Hg, representing a 37% reduction of IOP.8 In separate studies involving iStent inject in Canada and Australia, the mean number of medications was reduced by 42% (decreasing from 2.3 to 1.2 medications)9 and 65% (decreasing from 1.7 to 0.6 medications)10 at 1 year.
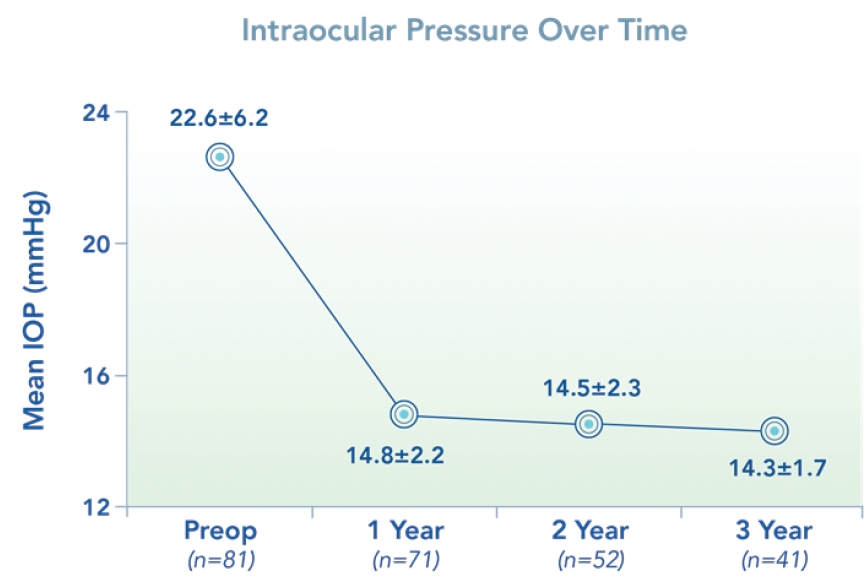
Figure 4. Long-term IOP reduction.8
Conclusion
Glaucoma treatment has shifted during the past 5 years, and, clearly, Glaukos remains a leader and pioneer in the MIGS market. iStent inject offers optometrists an excellent and highly rewarding opportunity to recommend the most micro-invasive and current treatment option for patients that are undergoing cataract surgery with mild-to-moderate POAG that is also supported with the vastest experience and data. It’s clinically proven IOP reduction may help prevent glaucoma progression which may in turn decrease your patient’s need for more invasive surgery and has the potential to simplify the management of your patient’s glaucoma.
The iStent inject fits seamlessly into optometric comanagement practices. With proven efficacy, an excellent safety profile, and predictable comanagement, the iStent inject is an excellent option for patients who have cataracts and mild-to-moderate POAG.
1. Data on file. Glaukos Corporation.
2. Asrani S, Zeimer, R, Wilensky J, Gieser D, Vitale S, Lindenmuth K. Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma. 2000;9:134-142.
3. Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008;17:350-355.
4. Market Scope 2017 and Medicare administrative claims data (Carrier 5% SAF) 2007-2010.
5. Data on file, Glaukos Corporation.
6. Huang A, Penteado RC, Papoyan V, et al. Aqueous angiographic outflow improvement after trabecular micro-bypass in glaucoma patients. Ophthalmol Glaucoma. 2019;2(1);11-21.
7. iStent inject Trabecular Micro-Bypass System: Directions for Use, Part #45-0176.
8. Hengerer FH, Auffarth GU, Curshmann M, Conrad-Hengerer I. One-year outcomes of implantation of second-generation trabecular microbypass stents in patients with open-angle glaucoma. Paper presented at: Annual Meeting of the American Society for Cataract and Refractive Surgery; April 16, 2018; Washington, DC.
9. Harasymowycz P. Single surgeon evaluation of second-generation trabecular micro-bypass stents in patients with mild to severe glaucoma. ASCRS 2018 Presentation.
10. Clement C. Outcomes with 2nd generation trabecular micro-bypass stents in patients with glaucoma: multi-center, multi-surgeon experience. APGC 2018 Presentation.



