There is increasing interest in the role of optometry in surgical care. Articles, meetings, symposia, and general discussion on the topic proliferate. Even the section of this magazine in which this article appears, CollaborativeEYE, emphasizes how much the role of the optometrist is evolving from primary eye care to surgical care. That said, much of the recent discussion in this area is about technological innovation or postoperative care. The time has come to change our optometric mindset and to integrate our- selves into the surgical process for better patient outcomes.
Fulfilling A Need
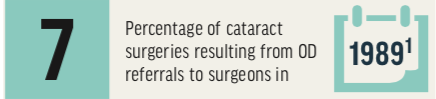
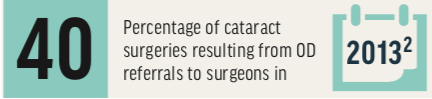
In 1989, a report from the Office of Inspector General of the US Department of Health and Human Services stated that 7% of cataract surgeries were the result of referrals to surgeons by optometrists.1 By 2013, industry data placed that figure at approximately 40%.2
It is estimated that the number of cataract surgeries performed world- wide will increase from more than 20 million in 2017 to more than 35 million by 2025.3 During that same time period, the supply of ophthalmologists is actually projected to decrease. The Association of American Medical Colleges projects that more than 6,000 additional ophthalmologists will be needed in the United States by 2020. In a 2017 report, the association projected a shortfall, citing increased demand for services exacerbated by difficulty increasing the number of high-quality surgical residencies.4
Couple increased demand and decreased supply of surgeons with decreased reimbursements, and the only option is to keep our surgeons in the OR where they can serve the most patients and be the most productive.
This future leaves eye care as a whole little choice. We have to change old models to become more efficient in serving patients. Serving patients means more than just surgery. It means evaluation, education, counseling, and providing decision-making assistance preoperatively, as well as providing what will be a tremendous number of postoperative care visits. Fortunately, optometry is perfectly positioned to step in to take on its role as part of the surgical team and fulfill this need.
Defending Relationships
The need for optometry to adapt to changes in patient volume and practice patterns provides a unique opportunity for the profession. We are facing a time when optometry practices struggle to differentiate themselves and retain patients. Integrating ourselves to become part of good surgical care will bring multiple benefits. Not only will it help to improve patient outcomes and facilitate patient throughput for surgical practices, it will also help optometry resist shifts in the health care market and the commoditization of eye care by potentially disruptive innovations such as online eye exams.
The FDA is considering a project in 2019 to allow sales of traditionally prescription drugs for chronic conditions such as high cholesterol, high blood pressure, asthma, and migraine to be guided by an app rather than a doctor’s visit.5 Although the future of telemedicine and app-driven health care may be bright, the fundamental patient relationships that make primary care positive for both doctor and patient must be defended.
Stepping Up
What steps can you take today to become more involved with your patient’s surgical care? It is actually much easier than you may think, as this is care we are already providing in some form.
First, when you refer a patient for surgery, make sure his or her ocular surface is ready for that surgery. The best surgery, laser assistance, and IOL upgrade can fall short of patient satis- faction due to a fog of ocular surface instability. Treat lid disorders, dry eye disease, and any corneal conditions preoperatively to optimize the ocular surface and maximize patients’ potential visual acuity and set them up for success.
Second, take a look at the patient’s keratometry (K) readings. We tend to over-focus on patients’ preoperative refractive (glasses) cylinder, which has little impact on postoperative induced astigmatism. If a patient is plano in each eye going into surgery, with glare complaints due to cataract and Ks of 42.00/44.00, he or she will not be happy with 2.00 D of postoperative cylinder and complaints of uncorrected glare.
This is a perfect example of why we as a profession need to become more involved in the surgical process. A simple assessment can tell us whether a patient is likely to develop astigmatism postoperatively. In addition to standard preoperative counseling, patients should be educated about what astigmatism is and why it is a factor for them before their procedure so that they can decide if it is something they would like to address.
Education before surgery is key; otherwise, the same conversation after surgery may be viewed by the patient as excuses after the fact. See Why Your Patients Deserve Their Optometrist’s Recommendations for Upgraded Cataract Surgery for additional insights.
The Big Picture
Our goal is to match patients’ long- term needs—not just what they think they want today, but what they will need for rest of their lives—to today’s technologies. Only you know your patients, their eyes, their needs, and what current treatment options could work for them. Make sure you are comfortable with the surgical options and IOL choices your surgeon utilizes. Do not get hung up worrying about pricing structures. You are not having a tech talk or a price discussion, you are educating patients so that they can make a value decision that capitalizes on the once-in-a-lifetime opportunity of cataract surgery.
Stabilize the ocular surface, match new technologies to the patient, and take ownership of the optometric role as a part of the surgical team to become more involved in cataract surgery. Taking these steps will help you to improve patient outcomes, set your surgeon and your patient up for success, safeguard your practice and our profession for the future, and adapt to potential market disruptions in the rapidly evolving health care environment.
- Office of Inspector General, US Department of Health and Human Services. Ophthalmology/Optometry Relationships Involved in Cataract Surgery. April 1989. oig.hhs.gov/oei/reports/oai-07-88-00460.pdf. Accessed January 8, 2019.
- Alcon. Data on file. December 10, 2013.
- Technavio. Global Phacoemulsification Devices Market 2019-2023. busi- nesswire.com/news/home/20181228005073/en/Global-Phacoemulsification- Devices-Market-2019-2023-Glaucoma-Surgery. Accessed January 8, 2019.
- Association of American Medical Colleges. 2017 Update. The Com-plexities of Physician Supply and Demand: Projections from 2015 to 2030. bit.ly/2017AAMC. Accessed January 8, 2019.
- U.S. Food & Drug Administration. Statement from FDA commissioner Scott Gottlieb, M.D. on new efforts to empower consumers by advancing access to nonprescription drugs. www.fda.gov/NewsEvents/Newsroom/PressAnnounce- ments/ucm613692.htm. Accessed January 16, 2019.