The prevalence of high myopia is increasing,1 which means educating patients with this condition about their refractive options is more important than ever before. The World Health Organization defines high myopia as a spherical equivalent objective refractive error ≥ -5.00 D in either eye.2 When speaking with patients, myopia control, contact lenses, glasses, LASIK, PRK, SMILE, and phakic IOLs all have a place in the conversation. Help your patients navigate their options by making the safest and best refractive recommendations for them.
For example, recommending corneal refractive surgery to patients with significantly high myopia can lead to disappointment. When ablating large amounts of tissue, the risk of reducing corneal integrity and increasing higher-order aberrations from the new corneal shape may be higher than acceptable to the surgeon or patient. A phakic IOL may be a suitable alternative in this situation.
SURVEYING THE PHAKIC IOL OPTIONS
The Visian ICL (STAAR Surgical) is currently the most widely used phakic IOL in the United States. A toric version of this lens (Visian Toric ICL, STAAR Surgical) was approved in 2018 (Figure 1). A second phakic IOL available in this country is the Verisyse IOL (Johnson & Johnson Vision in the United States; available elsewhere as the Artisan lens from Ophtec). The Verisyse is less popular than the Visian ICL in the United States because of differences in design; the former is a rigid PMMA lens that requires a large incision for implantation, whereas the Visian ICL is a foldable lens that requires a small incision.
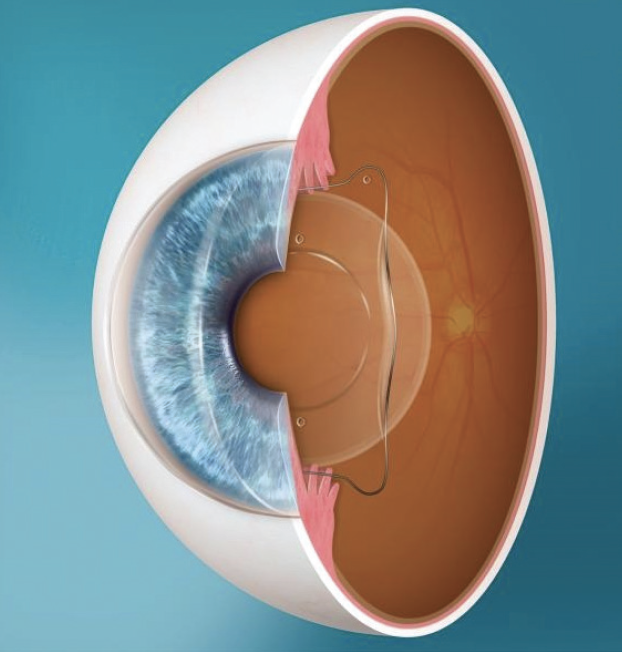
Figure 1. A Visian ICL placed in the ciliary sulcus.
Figure courtesy of STAAR Surgical.
Advantages of the Visian ICL (compared to laser refractive surgery) include reversibility; the induction of fewer dysphotopsias such as glare, halos, and starbursts; and a lower postoperative incidence of dry eye compared to LASIK.3
CANDIDACY FOR AN ICL
Candidates for a Visian ICL must be 21 to 45 years of age and demonstrate refractive stability within 0.50 D for at least 1 year before surgery. This ICL can correct -3.00 D to -15.00 D of myopia and ≤ 2.50 D of astigmatism at the spectacle plane. The ICL is also approved for use in eyes with > -15.00 D of myopia and ≤ 2.50 D of astigmatism at the spectacle plane. The anterior chamber depth must be at least 3.0 mm to allow safe implantation of the ICL without disturbing the iris, cornea, or crystalline lens.
Contraindications for this procedure include the following:
- An anterior chamber depth < 3.00 mm
- An anterior chamber angle less than grade 2 as determined by a gonioscopic examination
- An age older than 45 years
- Hyperopia.
PREPARING THE PATIENT
Before surgery, conduct a thorough evaluation of the patient that includes manifest and cycloplegic refractions, a measurement of white-to-white distance, slit-lamp biomicroscopy with gonioscopy, an endothelial cell count, and a measurement of anterior chamber depth. Closely evaluate the retina for tears or areas of significant pathology. In some instances, retinal treatment and clearance may be required before a patient may receive an ICL. Although ICL surgery itself does not significantly increase the risk of a retinal detachment, individuals with high myopia often have weak retinas and are predisposed to experience a retinal detachment.
If a patient is a good candidate for the ICL, the next step is to perform a laser peripheral iridotomy (LPI). During the procedure, two openings are created superiorly and located 90˚ apart, typically at the 11 and 1 clock positions (Figure 2). An LPI is usually performed 2 to 3 weeks before ICL surgery. An LPI helps to prevent the development of pupillary block and angle-closure glaucoma.
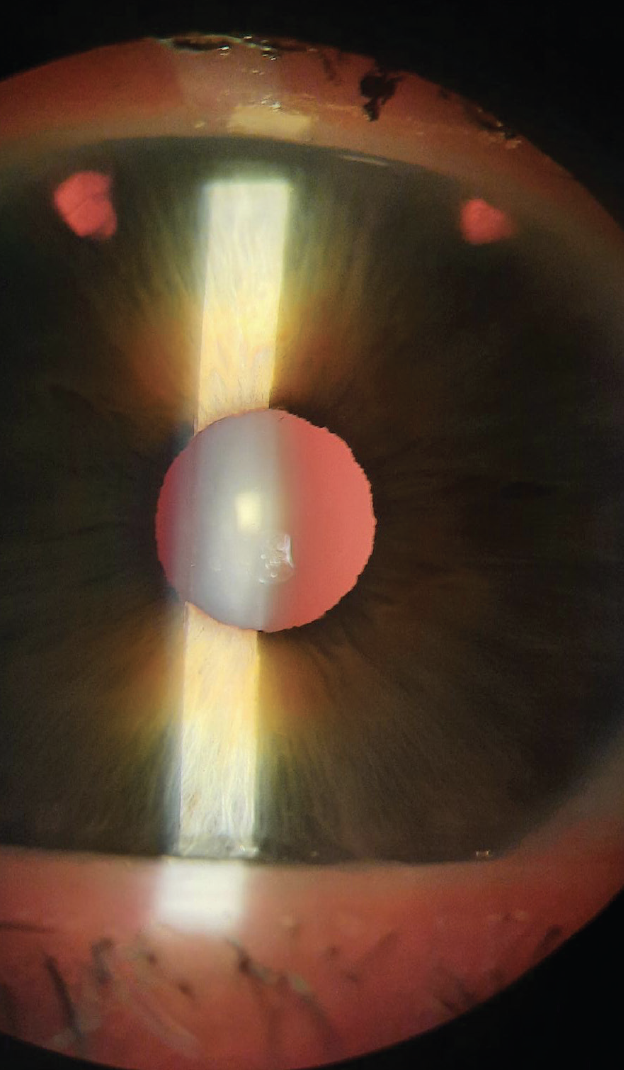
Figure 2. Patent peripheral iridiotomies performed at the 10 and 1 clock positions before ICL placement. This is an important evaluation for routine annual examinations before dilation.
VAULT
The surgeon carefully selects the size of the Visian ICL based on the white-to-white and sulcus-to-sulcus distances. Choosing the proper lens size ensures that the implant vaults appropriately (typically 250–750 µm) over the crystalline lens.
When measuring the vault, the slit beam is directed at a 30˚ to 45˚ angle to evaluate the corneal thickness as a baseline. The beam is then transferred to compare the depth between the back surface of the ICL and the front surface of the crystalline lens; this distance should be equal to or greater than the thickness of the cornea.
If the lens vault is too steep, the implant may rub the back surface of the iris, causing pigmentary dispersion syndrome. If the lens vault is too shallow, the implant may contact the surface of the crystalline lens and cause a cataract to form prematurely. It can be challenging to evaluate the vault because the ICL is clear. When in doubt, an anterior chamber OCT image can be helpful.
POSTOPERATIVE MANAGEMENT
Several postoperative visits with the surgeon are scheduled so that the lens position (ie, vault), IOP, and visual acuity may be checked. These visits generally occur immediately following surgery and at 1 day, 1 week, 1 month, and 3 months.
Patients experience a dramatic improvement in visual acuity during the first week after surgery. Many of them feel as though they can see well enough to drive on postoperative day 1.
The routine postoperative drug regimen includes topical drops to guard against infection and inflammation. Patients are instructed to wear an eye shield to bed to protect the eye during sleep for 1 week after surgery.
ARM YOURSELF WITH KNOWLEDGE
As the prevalence of high myopia increases, the number of patients who receive phakic IOLs is likely to rise as well. Collaborative care of these individuals may then go from a rarity to a more common practice.
Be ready to educate your patients on their refractive options and the importance of routine, yearly exams to ensure that their eyes are healthy. Individuals who are interested in refractive surgery but who are not suitable candidates for LASIK, PRK, SMILE, or a phakic IOL may meet the requirements for a refractive lens exchange based on their refractive error and age.
1. Holden BA, Wilson DA, Jong M, et al. Myopia: a growing global problem with sight-threatening complications. Community Eye Health. 2015;28(90):35.
2. The impact of myopia and high myopia: report of the Joint World Health Organization-Brien Holden Vision Institute Global Scientific Meeting on Myopia. World Health Organization. March 2015. Accessed November 11, 2021. www.who.int/blindness/causes/MyopiaReportforWeb.pdf
3. Kobashi H, Kamiya K, Igarashi A, Matsumura K, Komatsu M, Shimizu K. Long-term quality of life after posterior chamber phakic intraocular lens implantation and after wavefront-guided laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2014;40(12):2019-2024.
4. Nuria AS, Ortega-Usobiaga J, Beltrán-Sanz J, Druchkiv V, Llovet-Osuna F, Baviera-Sabater J. laser in situ keratomileusis and surface ablation in breastfeeding patients. Cornea. 2020;39(7):862-867.
5. Visian ICL product information. www.accessdata.fda.gov/cdrh_docs/pdf3/P030016c.pdf. Accessed January 11, 2022.





