Incremental improvements in technology during the past 2 decades have transformed cataract surgery into refractive surgery. Patients now expect outcomes rivaling those of LASIK and similar procedures, and, in many cases, these outcomes can be achieved. However, a sizeable minority of patients who have uneventful modern cataract surgery are ultimately unhappy with their visual outcome. Patients may achieve 20/20 uncorrected VA, but poor vision quality, fluctuating vision, and ocular discomfort caused by undiagnosed or undertreated ocular surface disease (OSD) can derail the surgeon’s best efforts.
In the patient’s eyes, these symptoms represent a surgical complication. I continue to have patients tell me that they never had dry eye prior to their cataract surgery. As patient postoperative expectations grow, and the prevalence of dry eye increases, it is paramount that optometrists and ophthalmologists work collaboratively to identify and treat patients with perioperative OSD appropriately.
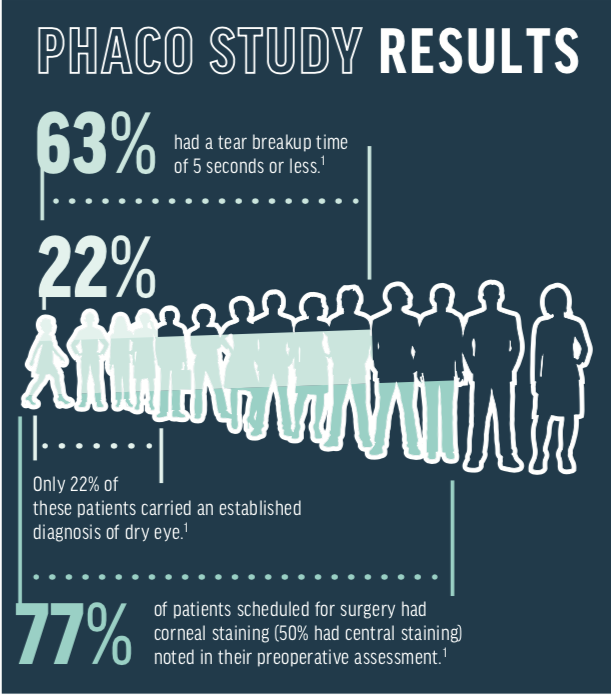
OSD is highly prevalent in the cataract population. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study evaluated patients presenting for cataract surgery. Remarkably, 77% of patients scheduled for surgery had corneal staining (50% had central staining) noted in their preoperative assessment, and 63% had a tear breakup time of 5 seconds or less. Only 22% of these patients carried an established diagnosis of dry eye.1 A more recent study by Gupta et al, utilizing point-of-care diagnostics, showed similar results — 80% of patients presenting for cataract surgery had either an abnormal ocular surface detected during slit-lamp examination, tear film hyperosmolarity, or increased tear matrix metalloproteinase-9 (MMP-9) levels on the ocular surface.2
Tear film hyperosmolarity is especially important as this contributes to tear film instability, which affects preoperative measurements used to determine IOL power. Epitropolous et al demonstrated that patients identified with hyperosmolarity of the tear film, regardless of the presence of symptoms of OSD, had greater variability in their keratometry readings and IOL calculations compared with those who had normal osmolarity.3A high-quality tear film is even more critical in patients opting for multifocal, accommodating, or extended depth of focus IOLs.
So how can optometrists and ophthalmologists work together to find and treat these patients before they move forward with a once-in-a-lifetime chance to improve their vision? Here are three key pearls that we use in my practice to achieve success.
Pearl No. 1: Identify and Treat OSD as Early as Possible
I am a strong advocate for the use of a dry eye symptom screening ques- tionnaire for every patient presenting for a comprehensive examination or surgical evaluation. In my practice, we use a modified Standard Patient Assessment of Eye Dryness (SPEED) questionnaire. If common symptoms such as fluctuating vision, eye fatigue, or burning are identified, the workup technician will obtain point-of-care testing including assessment of tear film osmolarity, tear matrix MMP-9 levels, and meibography. These tests have become essential for me to make an accurate diagnosis and develop a targeted treatment plan. Point-of-care diagnostics also streamline evaluation, generate additional revenue, and serve as important patient education tools.
After additional history and risk factor assessment is obtained, I perform a careful evaluation of the ocular surface after instillation of sodium fluorescein dye (and, often, lissamine green) via a saline moistened strip. It is critical that a measurement of meibomian gland function be included, and I generally use the Meibomian Gland Evaluator (Johnson & Johnson Vision) for this. Careful scrutinization of the ocular surface should be performed for all patients, regardless of whether they are symptomatic or not. Slit-lamp photography to capture images of anterior blepharitis, corneal and conjunctival staining, and other significant pathology can be valuable.
These images are helpful when educating relatively asymptomatic patients about their ocular surface abnormalities. I often tell patients that their condition is serious enough that we need to delay their surgery, but an image of their meibomian gland dropout or central superficial punctate keratitis tends to be even more effective. Waiting to properly identify and treat these issues only delays the patient’s ability to proceed with surgery. In most situations, treatment should be initiated by the primary care optometrist and the patient’s surface optimized before the referral is made.
Pearl No. 2: Preoperative Treatment Should be Aggressive
It is now accepted that dry eye is generally a chronic, multifactorial, immune-mediated inflammatory disease. In my experience, patients preparing for cataract surgery often need aggressive, multimodal therapy. This goes beyond standard therapy recommendations, such as lipidbased artificial tears, omega fatty acid supplements, warm compresses, and lid hygiene products. In patients with moderate to severe OSD symptoms and/or significant corneal staining, I judiciously prescribe loteprednol etabonate ophthalmic gel (Lotemax, Bausch + Lomb) as it works quickly by inhibiting T-cells on the ocular surface. A few weeks at two to four times a day dosing will benefit most patients. Additionally, in symptomatic patients or those who have minimally symptomatic disease but are interested in an advanced technology IOL, I routinely prescribe topical cyclosporine or lifitegrast (Xiidra, Shire). If patients don’t improve within 3 to 4 weeks with this regimen, their ocular surface is likely too compromised to seriously consider recommending a multifocal or extended depth of focus IOL.
Some patients with persistent keratopathy will require treatment with a cryopreserved amniotic membrane (Prokera Slim, Bio-Tissue) before surgery can be reasonably considered. In patients with poor meibomian gland function, I’ve had great success with the combination of microblepharoexfoliation (BlephEx, Scope Ophthalmics) and vectored thermal pulsation with LipiFlow (Johnson & Johnson Vision). In my satellite offices, I’ve also started to incorporate treatment with iLux (Alcon) as an alternative option for clearing meibomian gland obstructions.
Finally, addressing the lid biofilm with a lid cleansing agent is helpful in controlling symptoms and reducing bacterial load that may increase the risk for postoperative endophthalmitis. I generally favor agents containing hypochlorous acid as they are effective and well-tolerated.
Pearl No. 3: Briefly Delaying Surgery Until the Ocular Surface is Stabilized is in the Patient's Best Interest
Educate patients that dry eye is a visual disorder and that ignoring it will potentially compromise the results of their surgery. A pristine ocular surface will also improve their chances of being a candidate for an advanced technology IOL. Dry eye signs and symptoms may worsen temporarily with any ocular surgery, but aggressive preoperative management will help minimize this risk. And if a patient makes it to the surgical evaluation with undiagnosed or undertreated disease, ophthalmologists should resist the temptation to proceed with surgery until this has been rectified.
Avoid Suboptimal Cataract Surgery Outcomes
OSD is the number-one cause of suboptimal cataract surgery outcomes. With appropriate screening and diagnostic protocols, combined with aggressive treatment and a brief delay in getting to the OR, it certainly doesn’t have to be.
- Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.
- Gupta PK, Drinkwater OJ, VanDusen KW, Brissette AR, Starr CE. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evalua- tion. J Cataract Refract Surg. 2018;44(9):1090-1096.
- Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Ptvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015;41(8):1672-1677.






