Part I: The Future of Cataract Care

A New Model of Care
The demographics of our population are changing. People are living longer and are staying active later in life compared to previous decades. This brings an increased need for health and eye care, as the population requires functional vision for a greater number of years than in the past. As the Baby Boomer generation ages in the next decade or two, an overwhelming number of people will need surgical intervention, and older patients will need high-level care.
Advances in cataract technology can bring patients greater satisfaction than ever before. However, making the most of this technology requires changes in the way we diagnose, treat, and manage our patients. The ocular surface must be optimized in order to select the correct lens power and provide the patient with the best postoperative outcomes. With choices to be made, time must be taken to educate patients regarding their options. Finally, greater insight into a patient’s lifestyle and personality may make a big difference in what option is recommended.
Unfortunately, with the number of patients increasing and each one requiring increased time and attention, we also have fewer ophthalmologists graduating. Simply put, the upcoming supply of medical doctors is not large enough to treat the demands of an ever-growing population of cataract patients. A new model of care is needed to meet the needs of patients.
An Ideal Relationship
The best way to meet the needs of our patients is through a collaborative, patient-centered approach between MDs and ODs. As in most relationships, “ideal” means different things to different people. However, certain elements should be present in any collaborative relationship.
When establishing a working relationship between a surgeon and an optometrist, each party needs to be fully aware of and on board with what is expected of him or her. Each office should know how much of the patient’s care they will be covering, when the patient should be referred, and keep lines of communication open between the offices and the patient. Referrals can go both ways, with optometrists referring to surgeons for procedures and surgeons referring to optometrists to provide contacts and spectacles for those patients who will still require them.
In an ideal relationship, ODs can help relieve the burden cataract surgeons face due to their dwindling numbers and increasing patients. Prior to surgery, referring optometrists can help ensure optimal outcomes by addressing pathology such as ocular surface disease (OSD). As many of our cataract-age population likely suffer from at least moderate dry eye disease, there is a vast need for our referring doctors to identify it, discuss it, and start the treatment process.
Along those lines, the OD can also help prepare the surgeon by sharing preoperative notes detailing as much information about the patient as possible. ODs often treat the same patient for years, and any guidance regarding a patient’s personality, sensitivities to change in spectacle and/or SCL adjustments, visual goals, job-related concerns, and other issues is vitally useful in helping surgeons choose the best lens option for the patient. There are many great options for patients, but not all options will work for all patients.
An increased number of refractive options, some of which incur additional expense, means that that patients must be prepared to make both vision-related and finance-related decisions. These decisions cannot be made within a single appointment. In my experience, patients that are introduced to the concept of surgical and lens choices early in the process are much more likely to be content with their surgical care and outcomes.
We are living in a very exciting time with technology that continues to advance. Ophthalmology is such a unique field. It is truly the only field in all of medicine that does everything from primary care, to refractive nonmedical care (contacts and glasses), to the highest level of surgical care. There is a huge breadth of different types of services for patients that cover the spectrum in terms of needs, and these services should be delegated to those who can perform them best. By working together, we can ensure our patients are receiving the best possible care.
Part II: Establishing Collaborative Care Relationships

Various Models of Care
With the increased need to optimize the ocular surface and educate patients prior to cataract surgery, many surgeons and optometrists have decided the best way to meet the needs of their patients is to form joint practices. Working together in a single practice allows for a seamless division of tasks that optimizes everyone’s time and brings superior outcomes for the patient. However, joint practices are not the only effective way to perform collaborative care. In addition to the optometrists within our practice, we also collaborate with an extensive referral network.
Our director of optometric services builds and maintains relationships with each of our referring optometrists. This includes going out into the community and meeting the optometrists, organizing educational opportunities so that we are all on the same page, and personalizing each relationship so that the referring doctor is managing the cataract process to the degree that they are individually comfortable. Some optometrists want to engage in the entire process, from education and ocular surface optimization to seeing the patient on the first day postoperatively. This is particularly useful when the patient is located far from our office and returning for visits is difficult. Trust and confidence between the providers is essential in these relationships and once that it established, we respect each other’s wishes. Some optometrists prefer us to monitor the patient for the first month postoperatively, and we do that. We carefully define the roles ahead of time, and I have frequent, direct conversations with all referring providers so that the patient is always provided the highest level of care.

Getting on the Same Page
Education
Trust, respect, and a smooth patient experience depend on great communication and a shared concept of the ideal outcome (Figure 1). Patients should receive a consistent message from everyone involved in their eye care, and getting to that point requires joint educational opportunities. Our referral services team meets with our referring optometrists multiple times a year to discuss the latest research, technologies, tools, and outcomes.
Figure 1. An example of a Patient Referral Request Form, which can help ensure a smooth patient experience.
A variety of meeting formats work best for us:
- Education seminars that focus on refractive/cataract surgery are hosted roughly twice per year (Figure 2). These instructional courses provide the latest information and allow the optometrists to collect CE credits.
- Dinner roundtables are more intimate, with a few internal doctors meeting with a handful of referring partners around a specific topic with plenty of time to discuss nuances.
- Workshops/Wet labs are hands-on opportunities to test out new technology following a brief lecture. These are particularly useful to cover dry eye disease; external collaborating care providers can test each other’s tear osmolarity, examine meibomian glands, and get a real grasp of the importance of diagnosing and treating ocular surface issues prior to referring a patient for cataract surgery.

Figure 2. Education seminars that focus on refractive/cataract surgery are hosted roughly twice per year.
In addition to more formal educational opportunities, we routinely share how we are doing. Cataract surgery outcomes are tracked meticulously, and stratified based on lens type. Shared both internally and externally, this transparency gives our referring partners confidence both in the surgeons as well as in the technology that we are using. They see the high patient satisfaction rates with astigmatism correction and extended-depth-of-focus IOLS for the surgeons they are sending their patients to.
Expectations
Preparing the ocular surface can be the biggest holdup prior to cataract surgery, which is why we heavily stress the importance of diagnosis and treatment of dry eye disease by the primary eye care provider. A significant number of our educational reunions are focused on this topic, and we directly challenge referring doctors to address it. This is reinforced by specifically asking on the patient referral form if the ocular surface is cleared for cataract surgery.
While it does not cause the same delay, lack of patient education regarding the options can make the process much more stressful for the patient. If they have not been informed in advance that they will have to choose between covered technology and more advanced options with an out-of-pocket cost, this revelation can be stressful and result in mistrust. We encourage our referring partners to initiate this discussion and document what option each patient may be interested in (Figure 3).
Figure 3. Brochures help explain the different options to patients.
On the other side, all ODs should expect an open line of communication with the surgeons to whom they refer patients. While we have a dedicated liaison team which helps build the relationship, our surgeons are also readily available to discuss patient history, preferences, or concerns with their referring doctors.

The Sum is Greater Than the Parts
The single most important concept in a MD/OD collaborative relationship is that patient care comes first, and we are all looking out for the patient’s best interest. We want our patients to understand the different risks and benefits of various lenses. We strongly believe that multiple touch points in their education is important for patient understanding and realistic expectations.
For patients with astigmatism, it is easy to convey the advantages of a toric IOL. For patients who are considering a presbyopia solution, there is much more to consider. We strongly believe that the Symfony extended-depth-of-focus lens (Johnson & Johnson Vision) provides the best quality of vision at distance and also very good intermediate and some near vision. But we want to make sure that patients are going to be happy with their selection. Optometrists have long-standing relationships with patients and have insight into visual demands, concerns, and personalities that they have gathered over a lifetime of caring for this patient that I cannot gather in a single appointment. I depend heavily on this information when recommending an IOL.
The recent emergence of the impact of ocular surface disease (OSD) on cataract outcomes has really made the OD/MD relationship more important than ever. The impact of OSD on cataract surgery simply cannot be overstated; it impacts lens calculations, patient comfort, and postoperative vision. A referring optometrist who understands this, has diagnosed OSD, and taken the steps to improve the ocular surface has prepared the patient for the best outcomes possible following cataract surgery.
I am looking for partners that have the same standards and ethics I have and who will bring a level of expertise that will help me improve my patient care. I find this is rather easy to do, and I work with many referring optometrists that have helped me improve patient care.
Part III: Evaluating a Cataract Patient for a Premium Outcome


Collecting Valuable Data and Comanaging Patients
Anatomy of an Exceptional Workup
Marc R. Bloomenstein OD, FAAO: Our goal is to marry patients with a lens capable of achieving what they want to accomplish. The first step of a good examination is to understand what patients want to gain, and then educate them on their best options to attain the desired outcome—whether that is total freedom from glasses, near vision, good intermediate vision for computer work, distance vision for driving, or a combination.
We recognize that a healthy ocular surface is probably the most important marker in determining successful visual outcomes. Compromised tear film can deteriorate image quality due to light scatter, which deteriorates retinal image quality by as much as 20% to 40%.1 Further, these irregularities may produce higher-order aberrations (HOAs)2 increases and decrease visual acuity between blinks.3 Adding to this concern is that cataract surgery may cause or exacerbate dry eye that may have been present prior to surgery.4 In my experience, these factors all affect postoperative visual outcomes, recovery times, and overall patient satisfaction.
Every patient in our practice undergoes an examination of the ocular surface and retina, which includes topography. The examination includes osmolarity testing to prove homeostasis and normal tear quality, and conjunctival staining to locate any significant dry spots on the cornea. If we detect any signs of decreased tear function, we measure meibum secretion levels by looking at lid margins and the meibomian glands. We proceed to treat anatomical changes to the lids that would increase tear evaporation or decrease homeostasis prior to surgery to ensure the optimal outcome.
Cynthia Matossian, MD: Premium outcomes start with a healthy ocular surface. For every cataract consult, we conduct a modified version of the Standard Patient Evaluation of Eye Dryness (SPEED) survey, which we built into our electronic medical records so screening technicians cannot skip these questions. A positive response to any of these questions—“Does your vision fluctuate? Do your eyes feel tired? Do they feel gritty and grainy, or do they water?”— merits tear osmolarity (TearLab) and InflammaDry (Quidel Corporation) testing. The technicians are empowered to perform these two point of care tests prior to instilling any drops into the eye. We follow this with a refraction. Then, while the eyes are dilating, we perform meibography using the LipiView II Ocular Surface Interferometer (Johnson & Johnson Vision). Thereafter, the patients watch a video playlist on cataract surgery in the examination room that has been curated to educate them about cataract surgery, procedures, implant options, astigmatism, and presbyopia correction.
By the time I enter the examination room, the digital images are up on the monitor and ready for me to evaluate. I discuss gland function and perform a fundus and slit-lamp examination on the patient. I always utilize both lissamine green and fluorescein because each vital dye provides different information: lissamine green highlights conjunctival disease, whereas fluorescein identifies more corneal pathology. Then, the conversation with the patient starts. This process allows us to consistently and properly evaluate each patient for upcoming cataract surgery.
Comprehensive Topographers Lay the Groundwork for the Best Outcomes
Dr. Bloomenstein: Topographical mapping of the eye is paramount to achieving the best outcome and is an essential tool in any optometric examination. When considering cataract surgery, it is important to identify uncontrolled disease states as well as to know how much astigmatism and irregularity occurs on the cornea. Topography also elucidates hidden dry eye problems we cannot see (Figure 4), and it can also give us a good indication of whether or not there is symmetry within the front of the cornea. A patient’s starting topography gives us direction for what road we want to take when talking about different IOLs. Obviously, refraction is important, but when a patient is not seeing optimally we must rule out the surface of the cornea as the source of the decrease in vision. This will then lead to more detailed evaluation of the lens, macula, and other potential long-term complications.
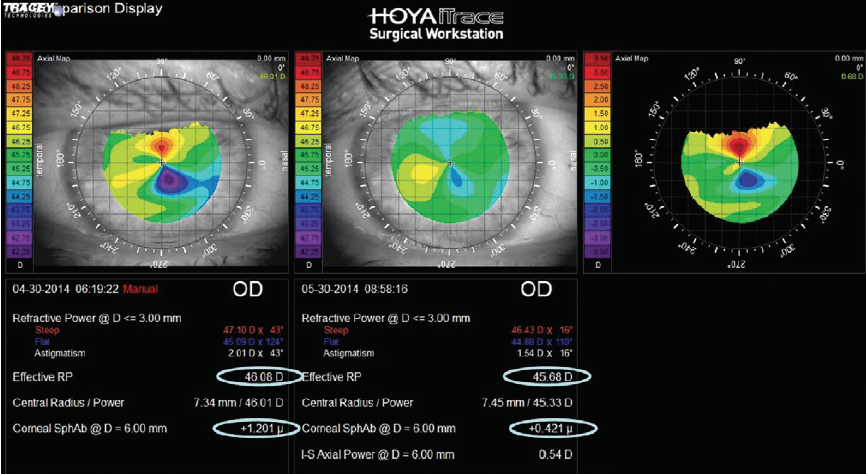
Figure 4. Placido disc images of a patient before and after dry eye treatment.
Dr. Matossian: I love my OPD-Scan III (Nidek), which integrates a wavefront aberrometer and a topographer; it is the one instrument besides a biometer that I cannot do without to plan for successful cataract surgery. In approximately 1 minute and with no discomfort to the patient, the technician is able to collect a treasure trove of valuable data. The OPD is easy to use with a relatively short learning curve for technicians; they simply take a picture of one eye, have the patient blink a few times, then capture the image from the second eye.
The OPD generates a huge amount of information including the internal, external, and axial maps; lenticular and corneal astigmatism; point-spread function; pupil diameter under mesopic and scotopic conditions; angle alpha and kappa to tell me about the physiological alignment of the optical elements; the amount and type of HOAs, including the corneal spherical aberration; and the root mean square (RMS) dioptric value of those aberrations to project outcomes. I amalgamate all of these data and then make a customized recommendation for each patient.
Shared Documentation Between Care Providers
Dr. Matossian: Preparing and planning for successful cataract surgery involves collaboration and consistent messaging between opticians, optometrists, surgeons, technicians, and office staff. We have to become a cohesive team to deliver the best outcomes for our patients.
My practice provides an integrated care approach, with our own comanaging optometrists performing all comprehensive eye examinations and postoperative monitoring, and medical doctors handling the surgical component. For those patients referred to us from an outside comanaging optometrist, we receive the medical records via fax or electronically. After the surgical component is complete, these patients return to their referring optometrist for follow-up care.
It is key to understand that everything that happens in the optometrist’s practice supports and prepares the patient for the surgical procedure. An optometrist aligned with a surgical center is a partner in the patient’s journey and can educate and prepare patients for upcoming steps and choices. For instance, a patient who requests an implant that may not be an ideal option for them will not be blindsided in the surgeon’s office if they arrive well educated. To engage in this type of discussion with patients requires appropriate diagnostic equipment to evaluate the tear film, cornea, and macula.
Dr. Bloomenstein: My responsibility as an optometrist is to learn the trends of the surgeons and alert them to the proclivities of patients. Typically, I have known patients longer and have background information that a surgeon cannot obtain from a single visit in a busy practice. My insight on a patient’s personality and lifestyle can help the surgeon manage patient expectations and tailor the discussion to satisfy the patient’s needs.
Part IV: Ocular Surface Disease Diagnosis and Management


A Surgeon and an Optometrist Provide Their Perspectives
The prevalence of ocular surface disease (OSD) is staggering, with some studies estimating the number of sufferers at nearly 55 million,5 many of whom go undiagnosed. The causes of such a widespread disease vary. The increasing use of screen-based technology and side effects from popular medications6 are certainly factors, and increasingly, younger people are experiencing dry eye along with the traditionally affected senior population.
The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO)7 study confirms that the incidence of dry eye in cataract surgical patients is higher than anticipated. Of the 136 patients (272 eyes), 60% had never complained of dry eye symptoms, yet nearly 80% demonstrated some level of ocular surface disturbance. PHACO reported tear break-up time of less than 5 seconds in 63% of patients; 77% showed positive staining; 50% had positive central corneal staining; and 18% had Schirmer test scores of less than 5 mm. While the number of physicians who screen for dry eye prior to surgical procedures is increasing, many cases go undetected.
Optimizing the cornea is essential to achieving the best refractive results not only for cataract surgery but for any ocular surgery. We have a wealth of data demonstrating that a healthy ocular surface produces consistency in keratometry and lens calculations. Accurate readings are critical for correct IOL placement, proper lens power calculation, and satisfactory refractive outcomes.
Since the prevalence of OSD is so high, most patients who have cataracts almost always have coexisting OSD. We start patients on personalized regimens based on the level of disease detected. Our initial treatment protocol is to start patients on preservative-free artificial tears, oral Omega supplements, and a microwaveable moist heat eye mask. We call this combination our starter “Dry Eye Triad.” For patients with more advanced disease, we may stack any single or combination of the following options: cyclosporine (Restasis; Allergan), lifitegrast (Xiidra; Shire), LipiFlow (Johnson & Johnson Vision), or a short course of loteprednol etabonate ophthalmic gel (Lotemax; Bausch + Lomb). We explain the glaucoma-related side effects of steroids drops and emphasize that the prescription will not be refilled. Depending on the severity of their OSD, patients return between 2 and 4 weeks. If the surface is responding to the prescribed treatment and the tear film is more stable, we proceed to take the preoperative measurements.
Under no circumstances will we take preoperative measurements immediately following a typical cataract consult examination. Diagnostic steps such as Goldmann applanation with topical anesthetic drops, vital dyes, mydriatic agents for the dilated funduscopic examination, and the bright indirect ophthalmoscope all impact the tear film. We decouple the cataract consult from the preoperative testing visit. We feel that we simply cannot obtain reliable data when OSD is present or when the surface has been iatrogenically pummeled, so we wait until after the tune up. Once we are confident that the ocular surface is as optimized as possible, we proceed with our preoperative measurements with the Cassini Total Corneal Astigmatism (i-Optics), OPD-Scan III (Nidek), and biometry with the IOLMaster 700 (Zeiss). Although there is some overlap in testing, our preference is to cross-compare test results for accuracy and reliability. We then personally calculate each patient’s IOL power.
During my consult, we show patients their astigmatism, keratoconus, and LASIK flap patterns on the colored OPD axial maps (Figure 5). Patients can see their Placido disc image with irregular and warped mires demonstrating their dry eye disease and unstable tear film. We inform patients of their pre-existing disease and explain that even though we can “cure” their cataract with surgery, their OSD is chronic, requiring a lifetime of treatment. This helps set realistic patient expectations.
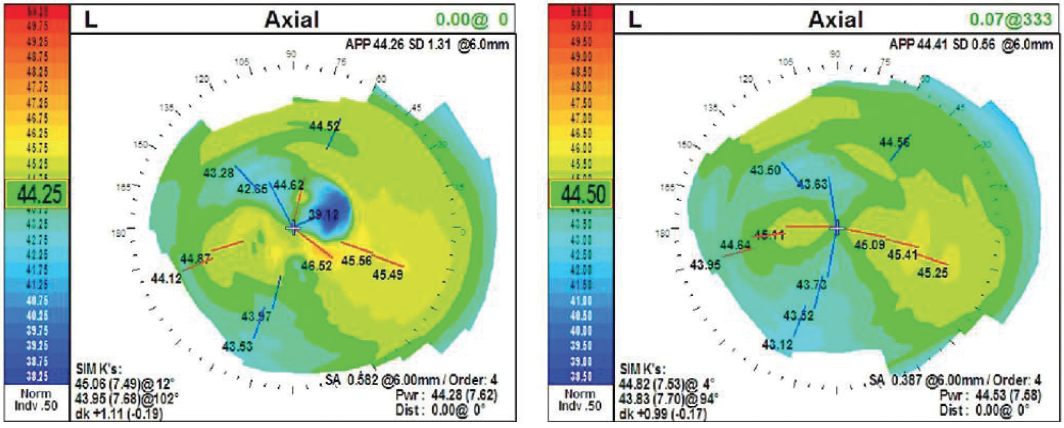
Figure 5. Dr. Matossian shares the colored OPD axial maps with her patients to educate them and set realistic expectations.
Untreated OSD May Delay Surgery
It is important to treat OSD prior to surgery to manage patient expectations regarding the timing of his or her surgery. There is no doubt of the effects of OSD on cataract surgery—from accurate metrics to patient comfort to increased function and refractive outcomes—the success of the surgery and the satisfaction of patients is highly dependent on the resolution of OSD prior to surgery. When a patient comes to us from an optometrist who understands this and has taken the steps needed to optimize the ocular surface, and then the patient hears us validate this action plan, the patient feels that his or her doctors share a mutual trust and care about him or her.
The surgeons and optometrists in our clinic appreciate working with referring ODs who screen and treat OSD prior to patients arriving at our clinic. If patients arrive without an optimized ocular surface, we very commonly have to delay their surgery with multiple treatments in order to optimize their ocular surface prior to their procedure. It is difficult for patients to understand why they were not diagnosed and treated by their referring optometrist, and it often causes anxiety because their surgery is being held up. However, when patients are referred from an optometrist who has apprised our clinic of their visual needs and treated pre-existing pathology, we immediately move to recommending the optimal IOL and scheduling surgery. By educating and working in tandem with referring optometrists, we create patient confidence and build a highly regarded practice.
Part V: Educating Patients About Their Options

Why Should Optometrists Engage in the Education Process?
Whether you agree with it or not, cataract surgery is now a refractive procedure. The current offerings in IOLs may enable patients to see as good as, and frequently better than, they did in their youth. But all of these options require decisions to be made, both on the part of the eye care provider and the patient. The earlier in the process patients are made aware of the options and the decisions to be made, the greater their confidence will be in their eye care providers, and the greater their satisfaction will be with the outcomes.
It is a mistake to think that because cataract extraction is a surgical procedure that all of the education should take place in the surgeon’s office. Optometrists provide the vast majority of comprehensive eye examinations to detect cataract, so that is where education should begin. Patients have to live with their surgical outcomes for the rest of their lives. Surgeons generally only see them once or twice. If patients are miserable or disappointed because they still need glasses postoperatively or if they are not the right personality type to deal with a presbyopia-correcting IOL, it is the optometrist who has to deal with them for the rest of their lives. The surgical journey should begin with their optometrist.
I like to start the education process with basic information on what is a cataract. The majority of patients think a cataract is a growth on the cornea, so I explain the basic anatomy, frequently using an eye model. I then explain how their surgery is done, and finally, I go into the lens options.
Femtosecond cataract surgery has brought another option to the table for how the capsulorhexis is performed, how the lens is broken up, how the incisions are created, as well as how astigmatism can be managed with arcuate incisions. Most patients do not realize that there are laser and manual options for performing all of these steps throughout the procedure. Telling patients about the different types of surgery early gives them much greater confidence in making an informed decision.
My best analogy to explain cataracts to patients is to tell them they have a lens Inside of a capsule, just like an M&M. We are going to leave the candy coating and swap out the chocolate filling with a new one.
— Marc R. Bloomenstein, OD, FAAO
When patients first come into our office, we have them fill out a questionnaire with information regarding their work, hobbies, feelings about wearing glasses, and other personality questions. This starts the discussion about what kind of lens will best suit them. For most people, a lot of work and free time is spent on a computer or a tablet, which are intermediate distance visual tasks. Previously, we could give patients distance vision and near vision for reading, but nothing for intermediate. In addition, because of the way these older lenses were structured with the two focal points, patients frequently had significant halos and glare.
Now we have extended-depth-of-focus lenses that may provide good, clear, crisp vision at distance and intermediate and still improve near vision. I tell my patients they still may need a pair of +1 readers for smaller print, but their vision will be excellent for most daily tasks. In my experience, these lenses elongate the light, truly decreasing the halo, glare, and night vision issues that we used to see. In addition, the lens is available in a toric version as well so we can take care of a patient’s astigmatism at the same time. The superiority of these extended-depth-of-focus lenses should relieve optometrists of the hesitations they may have had in the past about recommending presbyopia-correcting lenses to their patients.
Tools Available
Fortunately, there are a lot of tools available for explaining all of the technicalities around surgical steps and lens options. Manufacturers have created a plethora of educational materials to help patients understand the choices they will need to make. There are animated videos that can be posted on your website and shown to patients when they are in the office.
There are also excellent and informative pamphlets for all of these topics. They are provided free from the manufacturer and require no work on the part of the optometrist to have them in their office to distribute to patients.
It is Worth the Time
If the majority of a patient’s experience—education and follow-up before and after cataract surgery—was with his or her optometrist, that is the person he or she is more likely to refer friends and family to in the future. When optometrists engage in the education process, it is better for the patient and their practice.
Part VI: Postoperative Management and Collaboration


Tips on Having Happier Postoperative Patients
Pearls From Dr. Bloomenstein
The postoperative course for a premium IOL should be identical to a standard IOL. The goal is to ensure that the lens is centered, that the patient is seeing well, and that he or she is healing properly. All of these things are accomplished regardless of the IOL. The difference with a premium IOL is that patients have a greater anticipation of what they should be able to do without the assistance of spectacles or contact lenses, so it is important for the optometrist to assure patients that what they are seeing is commensurate with the lens they have.
If we ask a patient if they are having problems, they will usually parrot back to us all of the anticipated postoperative occurrences such as halo around light. What I find more effective is to ask them what they are seeing with both eyes open. I always check binocular distance, reading, and then intermediate vision, and then I “tell” them how well they are doing. They may look at the chart and be discouraged that they cannot read to the very bottom, but only you know the level of improvement and the capabilities their new vision can withstand. For example, if a patient is seeing 20/30 in one eye and 20/25 in the other, they are most likely seeing close to 20/20 binocularly. Yet they may focus on the more blurred eye. Tell them they have met the expectations, rather than tempt them to say they have not.
A premium lens may also differ from a standard monofocal lens in terms of neuroadaptation. We know that adapting to these lenses requires a longer mental process, so remind patients that they are in a marathon, not a sprint, and continue to tell them they are doing well. Patients really look to the clinician to gauge how they are healing. Since most patients give a litany of complications they are noticing, it is hard to determine which are really problematic. Do not address all of the complications. If your patient is truly having problems, they will stop you before they leave and ask for a solution.
Doctors in charge of postoperative care should also know that a small amount of astigmatism or a cloudy posterior capsule will have a much more dramatic effect with a multifocal or extended-depth-of-focus IOL, and these patients may need a follow-up enhancement from the surgeon. Therefore, keep a closer eye on these patients for any small changes to the capsule.
Pearls From Dr. Devries
In past years, premium IOLs were more likely to be utilized on patients before they were properly educated and had their ocular surface prepared, and those often became really difficult patients for optometrists to manage. This may have led to optometrists dissuading patients from wanting premium IOLs. However, much of that has changed. The advantage to the optometrist being thoroughly invested in the preoperative preparation is that the outcomes are better, and patients are happier in their postoperative time.
The postoperative course for a multifocal or extended-depth-of-focus lens is physically almost identical to any standard lens, but there is more time required for the patient to go through neuroadaptation and learn how to properly utilize the lens. By telling them up front that this is a learned process, and that they will be better in a month than they are initially, you can set proper expectations of the time frame required for complete adaptation.
When to send the patient back to the referring OD depends on the medical stability of the patient and the comfort level of the individual OD. Thus, it remains important for both collaborating doctors to share information throughout the postoperative period. Surgeons need to provide the optometrist information on what lens was implanted, the target refraction, and if it is a toric lens, the axis it was placed on. They also need to know the day 1 postoperative results and what medications the patient is using (unless the MD is providing the day 1 care). Postoperatively, the optometrist needs to verify that the wound is secure, look for inflammation in the anterior chamber and that it is well formed as well as measure refraction, intraocular pressure, visual acuity, and look at the peripheral retina. At 1 month, the OD should check all of the previous items as well as look for cystoid macular edema. During the 3-month visit, repeat all previous checkpoints and add opacification of the posterior capsule. All of this information should be returned to the surgeon so that postoperative information is reviewed and is in both files.
- Tutt R,Bradley A,Begley C,Thibos LN. Optical and visual impact of tear break-up in human eyes. Invest Ophthalmol Vis Sci. 2000;41(13):4117-4123.
- Goto E,Yagi Y,Matsumoto Y,Tsubota K. Impaired functional visual acuity of dry eye patients. Am J Ophthalmol. 2002;133(2):181-186
- Montés-Micó R. Role oaf the tear film in the optical quality of the human eye. J Cataract Refract Surg. 2007;33(9):1631-1635.
- Roberts CW, Elie ER. Dry eye symptoms following cataract surgery. Insight. 2007;32(1):14-23.
- The Gallup Organization, Inc.The 2004 Gallup Study of Dry Eye Sufferers. Princeton, NJ: Multi-Sponsor Surveys, Inc; 2004.
- Moss SE, Klein R, Klein BE. Incidence of dry eye in an older population. Arch Ophthalmol. 2004;122(3):369-373.
- Trattler WB, Majmudar PA, Donnenfeld ED, et al. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye.Clin Ophthalmol. (Auckland, NZ). 2017;11:1423-1430. doi:10.2147/OPTH.S120159.
Independent educational supplement supported by

and











