A thorough preoperative evaluation helps to minimize complications after LASIK. This step also provides an opportunity to manage patients’ expectations. Ideal LASIK candidates are motivated but also have realistic expectations. Contraindications for the procedure include a history of keratoconus, ocular trauma, corneal dystrophy, diabetes, or an autoimmune condition; pregnancy; lactation; and keloids.
AT A GLANCE
• Microstriae tend to resolve on their own and do not require treatment; macrostriae are frequently a result of eye rubbing or mechanical contact and often require surgical intervention.
• Older age, previous corneal trauma, diabetes, and epithelial basement membrane dystrophy are risk factors for the development of a corneal epithelial defect during LASIK.
• Diffuse lamellar keratitis is rare and typically presents 1 to 2 days after LASIK. The differential diagnosis includes meibomian gland secretions, debris, and dryness.
Key components of the preoperative examination are the manifest refraction and cycloplegic refraction, dry eye testing, assessments of the anterior and posterior segments, measurements of pupillary size, testing of ocular dominance (important for monovision patients), and topography. Topographic evaluation includes looking for signs of keratoconus and pellucid marginal degeneration, back surface elevation, asymmetry between the eyes, and irregular astigmatism. When calculating the residual stromal bed, the following formula may be used: central corneal thickness – (110 µm for the flap + 17 µm for each diopter of ablation).
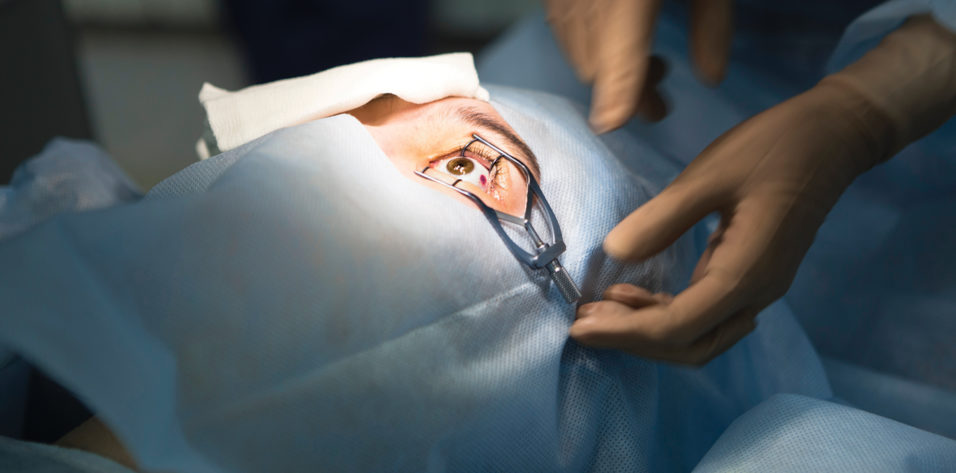
At Dougherty Laser Vision, we comanage patients with more than 300 referring optometrists. LASIK follow-up visits occur at 1 day, 1 week, 1 month, 3 months, 6 months, and, if needed, 1 year. The safety and efficacy of LASIK are excellent, but complications can occur, even when the best technology is used and the preoperative evaluation is thorough. This article provides an overview of eight potential post-LASIK complications.
NO. 1. UNDERCORRECTIONS AND OVERCORRECTIONS
Undercorrection is more common after primary LASIK than overcorrection, which is generally accepted by most surgeons. An undercorrection is more likely to occur in patients with high myopia, hyperopia, or astigmatism. Overcorrection most often occurs after a retreatment.
Undercorrections and overcorrections are often addressed with an enhancement procedure performed 3 months after the refraction stabilizes. The surgeon relifts the flap and performs a second ablation. When co-managing LASIK patients it is important as an OD to monitor the refraction at every postoperative visit. Generally, if the prescription is stable for at least two visits the patient can be referred back to the surgeon for the enhancement procedure.
NO. 2. DRY EYES
Some patients experience a decrease in tear production, which can cause a foreign body sensation, blurred vision, or ocular discomfort. Patients who have dry eye disease are not ideal candidates for LASIK surgery and may be better served by other refractive surgery options such as the implantation of phakic IOLs.
Caused by corneal denervation, dry eye is one of the most common side effects of LASIK. It is usually temporary. Treatment depends on dry eye severity. Options include preservative-free lubricating drops, collagen plugs, steroid therapy for a limited duration, lifitegrast ophthalmic solution 5% (Xiidra, Novartis International), and cyclosporine ophthalmic emulsion 0.05% (Restasis, Allergan).
NO. 3. NIGHTTIME VISUAL DISTURBANCES
The treatment of nighttime visual disturbances should address the root cause. Patients who experience glare and halos at night typically have pupils that dilate in reduced-light settings, but a residual refractive error can also cause these symptoms. Spherical aberrations typically occur in dim light when the pupil dilates larger than the area of the cornea that was fully corrected by the laser treatment. Brimonidine tartrate ophthalmic solution 0.1% or 0.15% (Alphagan P, Allergan) and low-dose pilocarpine are two options for managing large pupils. A thorough discussion of the potential side effects (eg, retinal detachment) should take place before pilocarpine is prescribed.
A decentered ablation can also cause nighttime visual disturbances. This complication is rare, thanks to the advanced tracking systems of modern laser platforms. Decentered ablations are diagnosed using topography. If the comanaging optometrist suspects an issue with the ablation, he or she should refer the patient back to the surgeon immediately.
Higher-order aberrations are more common after conventional LASIK methods compared to wavefront-guided LASIK procedures. Conventional LASIK takes only refraction into consideration, whereas wavefront-guided LASIK considers both higher and lower-order aberrations. A topography-guided retreatment may be performed to reduce higher-order aberrations. As the comanaging optometrist, it is important to look out for patients complaining of starbursts, halos, or multiple images after LASIK.
NO. 4. FLAP STRIAE
Small wrinkles or folds may be observed in the cornea after LASIK. Striae may be divided into two categories based on size. Microstriae are microscopic, superficial wrinkles in Bowman layer and/or the corneal epithelial basement membrane. They usually cause no visual symptoms. Macrostriae are full-thickness folds in the cornea that usually impair vision. Both forms of striae can be identified with retroillumination, and corneal staining with sodium fluorescein dye can show the magnitude of the folds.
Striae are a post-LASIK complication. Microstriae tend to resolve on their own and do not require treatment. Unless a patient is experiencing significant visual symptoms, observation is appropriate. Macrostriae are frequently a result of eye rubbing or mechanical contact, and these folds often require surgical intervention. In these cases, the ophthalmologist will relift the flap and smooth it with a surgical sponge.
NO. 5. EPITHELIAL INGROWTH
After LASIK, epithelial cells can migrate between the corneal flap and the stromal bed. Epithelial ingrowth typically occurs during the first 3 months after surgery, often in the first 1 to 2 weeks. The patient may experience a decrease in vision secondary to astigmatic changes from topographic alterations produced by the invading cells. A diagnosis is usually made during the slit-lamp examination, which reveals pearly white aggregates with a smooth outline (Figure 1). Nests of cells that cause whorl-like opacifications can also appear, usually close to the flap’s edge.
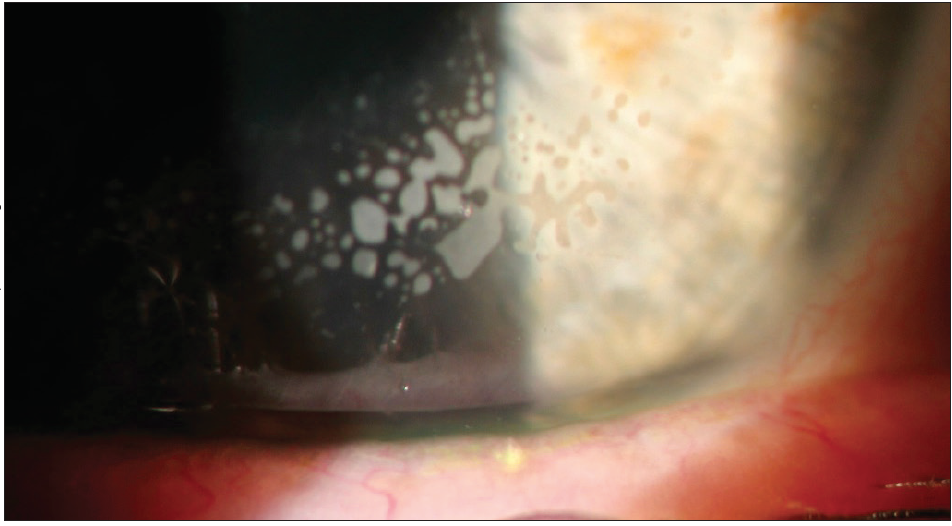
Figure 1. Epithelial ingrowth noted upon slit-lamp examination. Intralamellar epithelial cells with a whorl-like pattern, as seen here, are key to identification.
If the epithelial ingrowth is located away from the visual axis or pupil, the patient may be observed, and the complication may resolve on its own. If the epithelial ingrowth is visually significant or larger than 2 mm, then surgical intervention is required. This typically involves lifting the flap, scraping the epithelial cells, and placing a bandage contact lens.
NO. 6. CORNEAL EPITHELIAL DEFECTS
Older age, previous corneal trauma, diabetes mellitus, and epithelial basement membrane dystrophy are risk factors for the development of a corneal epithelial defect during LASIK. Treatment consists of the hourly administration of artificial tears, the application of lubricating ointment at night, and—for defects larger than 1 mm—the placement of a bandage contact lens to heal the defect and improve patient comfort.
NO. 7. DIFFUSE LAMELLAR KERATITIS
Diffuse lamellar keratitis (DLK) is a rare, noninfectious, sterile inflammatory reaction to antigens on the corneal interface. DLK typically presents 1 to 2 days after LASIK. Its location is usually superior, which means it is often missed if the eyelid is not retracted during the postoperative examination. The differential diagnosis includes meibomian gland secretions, debris, or dryness.
At the slit lamp, DLK is characterized by white, grainy cells underneath the LASIK flap interface (Figure 2). In its severe stages, DLK can cause corneal scarring, vision loss, and stromal melting. Patients with DLK often experience pain, foreign body sensation, photophobia, and blurry vision. Some, however, may offer no complaints, making it critical that ODs be vigilant for this complication during the early postoperative period and immediately inform the surgeon of any concerns.
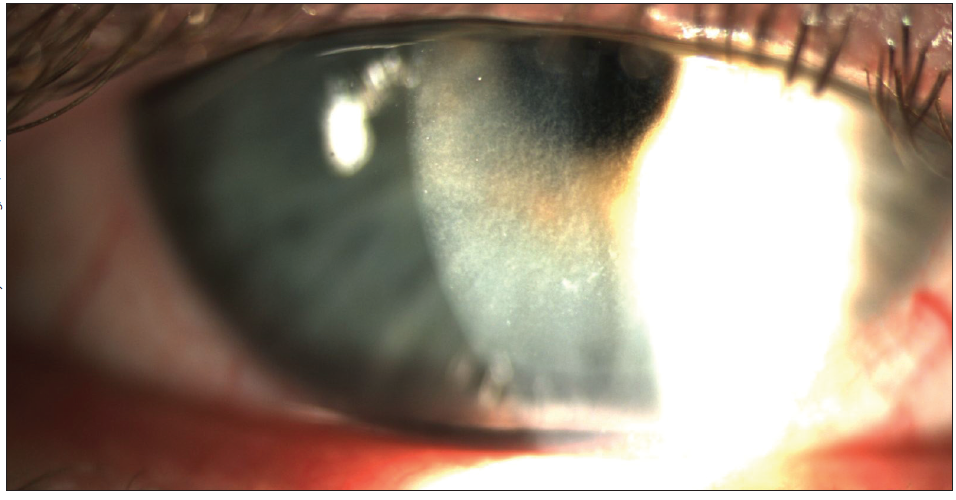
Figure 2. Diffuse lamellar keratitis identified by white, grainy bands of intralamellar inflammatory cells viewed by slit lamp.
DLK is treated aggressively with steroids, one drop administered every 1 to 2 hours. I generally prescribe prednisone acetate rather than difluprednate ophthalmic emulsion 0.05% (Durezol, Alcon). Difluprednate has been associated with pressure spikes1,2 and may cause a steroid response in some patients and should therefore be used with caution. If difluprednate is prescribed, IOP should be monitored carefully. After the initiation of steroid treatment, DLK typically resolves in 5 to 8 days. If the condition persists, the surgeon may lift the LASIK flap and irrigate the interface with balanced salt solution.
Early intervention for DLK carries a better prognosis.
NO. 8. CORNEAL ECTASIA
Corneal ectasia is a rare but devastating complication after LASIK. In terms of prevention, properly calculating the residual stromal bed (acceptable range, 250–300 µm) and assessing topography for asymmetry are critical components of the preoperative evaluation. Additional risk factors are young age, low preoperative corneal thickness, and high myopia.
Treatment for corneal ectasia mirrors that for keratoconus and pellucid marginal degeneration. Scleral contact lenses, rigid gas permeable lenses, and hybrid contact lenses can improve quality of vision. Intrastromal corneal ring segments can improve visual function. CXL can strengthen the cornea and halt ectatic progression. Some surgeons combine the placement of intrastromal corneal ring segments with CXL to stabilize the cornea and improve visual function. Penetrating keratoplasty is a last resort for visual rehabilitation. It is important for the co-managing optometrist to have a proper preoperative refraction noted and to discuss other refractive surgery options such as photorefractive keratectomy or a phakic IOL with patients who have thinner corneas.
KEEP AN EYE ON THE FLAP
As primary eye care providers, optometrists must ensure excellent pre- and postoperative care for LASIK patients. Effective communication between the optometrist and the refractive surgeon is essential in avoiding and managing post-LASIK complications. Assessing the flap with precision at every postoperative visit is critical to detecting complications early and managing them successfully.
1. Korenfeld MS, Silverstein SM, Cooke DL, et al; Difluprednate Ophthalmic Emulsion 0.05% (Durezol) Study Group. Difluprednate ophthalmic emulsion 0.05% for postoperative inflammation and pain. J Cataract Refract Surg. 2009;35(1):26-34.
2. Cable MM. Intraocular pressure spikes using difluprednate 0.05% for postoperative cataract inflammation. Assoc Res Vis Ophthalmol Ann Meet Abstr. 2010;51:1981.