As procedure-based treatments for the management of glaucoma become increasingly popular, optometrists will continue to play a vital role in the care of these patients. Against a backdrop of more normalized comanagement arrangements between ophthalmologists and optometrists, there are abundant opportunities to participate in the care of patients, with each stakeholder (especially our patients) deriving benefit.
Surgical Management of Glaucoma: Earlier Intervention With MIGS
With the safety profile of iStent inject (Glaukos) similar to that of cataract surgery alone, the favorable benefit-to-risk ratio has moved surgical intervention earlier in the care for many patients with mild-to-moderate primary open-angle glaucoma with cataracts and fits nicely in a collaborative care approach. This in turn has provided patients with an option for gaining long-term IOP control with the potential to decrease dependence on burdensome medications at the discretion of an eye care provider.1-3 In the pivotal trial, 75.8% of patients achieved at least a 20% reduction of unmedicated IOP at 24 months compared with baseline.1 At 3 years of followup, Hengerer et al found that patients had a mean IOP of 14.3±1.7 mm Hg.2 Clement reported an overall 65% reduction in mean number of medications.3
The iStent inject consists of two stents, each containing a central inlet and four side flow outlets. The stents are implanted through the trabecular meshwork 2 to 3 clock hours apart and deliver access to multiple collector channels and arcs of flow spanning 5 to 6 clock hours in total (Figure 1). Deliberately engineered to be no larger than necessary to optimize natural aqueous fluid dynamics, the iStent inject is the smallest known medical device in the world with a length of 360 µm and diameter of 230 µm. It is truly “micro” in scale.
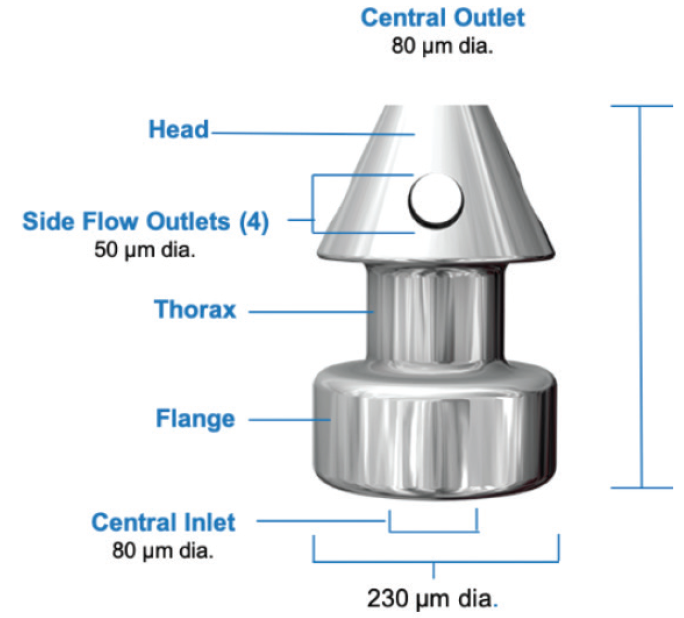
Figure 1. The iStent inject.
A Collaborative Approach to Glaucoma Management
The iStent inject is intended for use at the time of cataract surgery, thus it is paramount for optometrists to address this once-in-a-lifetime opportunity with their patients, as they are often their first-line eye care provider. Individuals with mild-to-moderate glaucoma constitute about 77% of the total glaucoma burden (Figure 2). In turn, as many as one-fifth of patients undergoing cataract surgery are prescribed at least one ocular hypertension medication.4
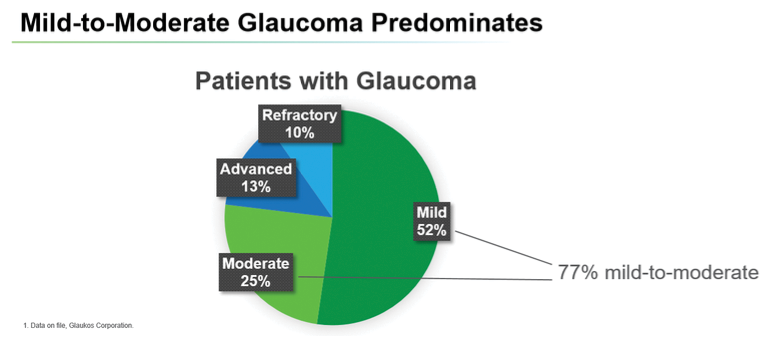
Figure 2. Individuals with mild-to-moderate glaucoma constitute about 77% of the total glaucoma burden.
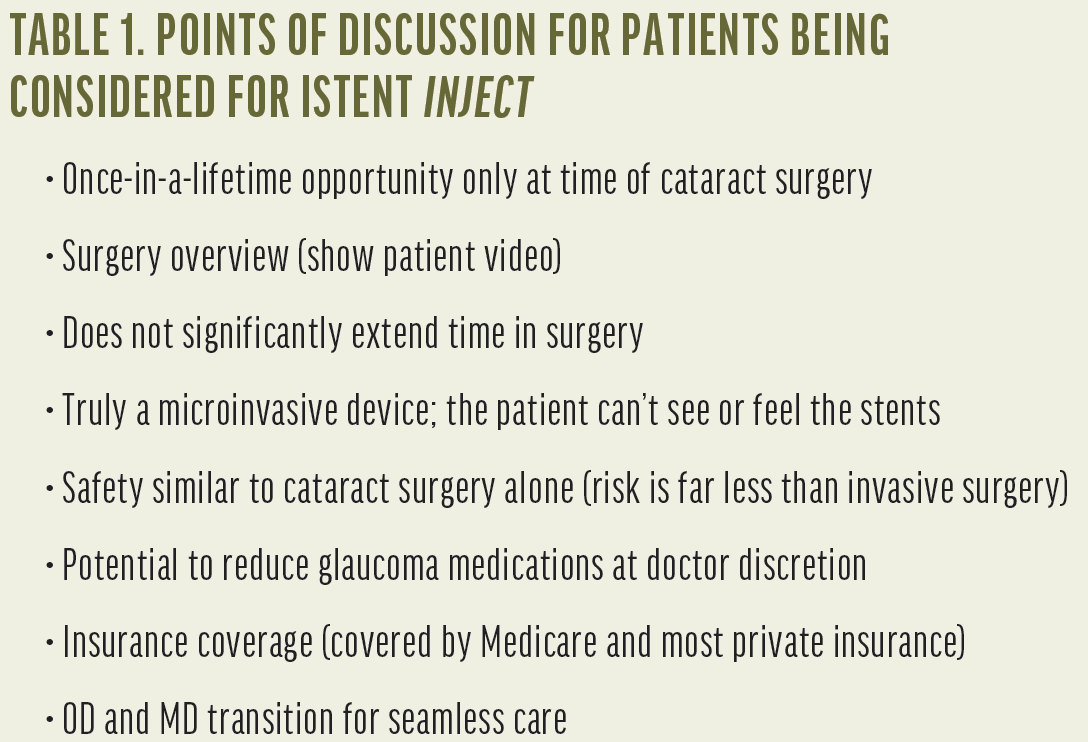
Any optometrist who is engaged in collaborative eye care is already well-equipped to participate in the comanagement of iStent inject. Evaluating a cataract patient with glaucoma for an iStent inject procedure may involve a careful slit lamp gonioscopy evaluation, recording IOP readings, visual field testing, optic nerve assessment (preferably with OCT), pachymetry, and a dilated fundus examination. We’ve found that patients who are informed about iStent inject before being referred for a surgical consultation have better expectations and appreciate learning about the possibility of treating their glaucoma at the same time as their cataract surgery (Table 1). Optometrists can optimize patient education due to the longstanding knowledge of their patient’s eye history and glaucoma management goals. Patients are comfortable learning about iStent inject from their optometrist, as a certain level of trust has often been established over time. It is, in turn, encouraging when the ophthalmologist corroborates presurgical discussions had with an optometrist.
The postoperative management of iStent inject offers a predictable and consistent comanagement process very similar to that of cataract surgery and also delivers similar visual acuity potential and visual recovery. In our collaborative approach, the patient is typically seen by the optometrist on day 1, although some practices prefer to transfer care at week 1; this varies by practice and patient. On day 1, we carefully monitor IOP and review with the patient their use of antibiotics and gradual tapering of steroids. Vision may be slightly decreased and mild edema may be present at the site of the wound due to the procedure. There may be scant red blood cells present in the anterior chamber; this typically resolves by the week 1 visit. When gonioscopy is performed, the position of the stents should be visualized. At day 30, IOP is assessed and has typically normalized. If the pressure allows, we may start withdrawing glaucoma medications one at a time. Contrarily, some practices halt glaucoma medications at time of surgery and choose to add them later, if necessary.
In our experience, by day 60, the anterior chamber is quiet, and patients have achieved their new normal visual acuity. We recommend performing a baseline glaucoma evaluation around day 90 to fully assess the effects of the intervention and to set a new target IOP.
Conclusion
For the patient with a cataract and mild-to-moderate primary open-angle glaucoma, phacoemulsification with placement of iStent inject presents an opportunity to address equally prominent concerns. There is potential to reduce, if not eliminate, at the discretion of an eye care provider, the need for medications that patients find costly, burdensome, and disruptive to daily life activities.
Implementing protocols for evaluating patients for the iStent inject and educating patients about their glaucoma treatment options does not require much deviation from cataract surgery. We have found that informing patients about the potential to undergo a microinvasive glaucoma surgery procedure, and making a specific recommendation to the referring surgeon, actually inspires confidence and builds trust that makes patients want to return to the practice—and potentially even refer other patients.
The model of collaborative eye care has evolved, and the idea of having the optometrist perform the preoperative assessment and follow the patient after surgery has become more commonplace. Indeed, any optometrist who is comfortable with comanaging cataract cases is already well-equipped to also comanage patients who are candidates for the iStent inject.
1. Samuelson T, Sarkisian S, Lubeck D, et al. Prospective, randomized, controlled pivotal trial of iStent inject trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019. [Epub ahead of print]
2. Hengerer FH. Personal experience with second-generation trabecular micro-bypass stents in combination with cataract surgery in patients with glaucoma: 3-year follow-up. Presented at: ASCRS 2018.
3. Clement C. Outcomes with 2nd generation trabecular micro-bypass stents in patients with glaucoma: multi-center, multi-surgeon experience. Presented at: APGC 2018.
4. Data on file. Glaukos Corporation.
5. Asrani S, Zeimer R, Wilensky J, et al. Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma. 2000;9(2):134-142.
6. Sleath B, Robin AL, Covert D, et al. Patient-reported behavior and problems in using glaucoma medications. Ophthalmology. 2006;113(3):431-436.
7. Leung E, Medeiros F, Weinreb R. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008;17(5):350-355.
iStent inject is a trademark of Glaukos. © Glaukos 2019. All other brand/product names are the trademarks of their respective owners. PM-US-0124



