Like many refractive surgeons, I was excited when corneal inlays became available in the United States. After all, the potential pool of candidates is enormous—approximately 100 million presbyopes in this country alone. I soon realized, however, that most of these potential patients simply are not visiting ophthalmology practices. Generally speaking, these individuals have seen fairly well throughout their lives. Their main exposure to eye care is purchasing over-the-counter readers at the drugstore. They do not understand that refractive surgery is an option for addressing the change in their vision, and frankly, many of them would hesitate to undergo surgery when they have had perfect eyes.
Unable to reach that target market for corneal inlays, my attention turned to the patients with mild to moderate hyperopia or myopia who are presbyopic and presenting to my practice with an interest in refractive surgery. In the past, the options we discussed were laser vision correction with the need for a pair of reading glasses postoperatively (a disappointment to many) or monovision. Today, I offer them the choice of LASIK combined with a corneal inlay to provide them with great distance and functional near vision. I find that this strategy increases the wow factor for a population already motivated to undergo refractive surgery.
CASE EXAMPLE
A 50-year-old engineer presented to my practice for a LASIK evaluation. The patient had a bilateral refraction of -4.00 D. He had tried contact lens monovision without success and wanted to maintain binocular distance vision and stereo acuity.
I explained the patient’s three options to him:
1. LASIK to correct the distance vision in both eyes and the use of reading glasses postoperatively;
2. LASIK monovision; or
3. LASIK combined with a corneal inlay.
The patient decided to pursue the combined procedure. Because the shape-changing inlay (Raindrop Near Vision Inlay [available at the time]; ReVision Optics) mimics a monovision experience, I felt the aperture inlay (Kamra; SightLife) would be more successful in this case, based on the patient’s history.
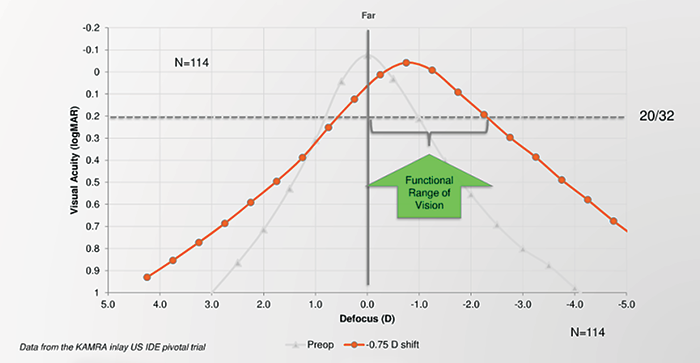
For the patient’s LASIK refractive goal, I targeted his dominant right eye for distance vision and his nondominant left eye for a refraction of -0.75 to -1.00 D. The aperture inlay was placed in his nondominant eye (Figure 1).
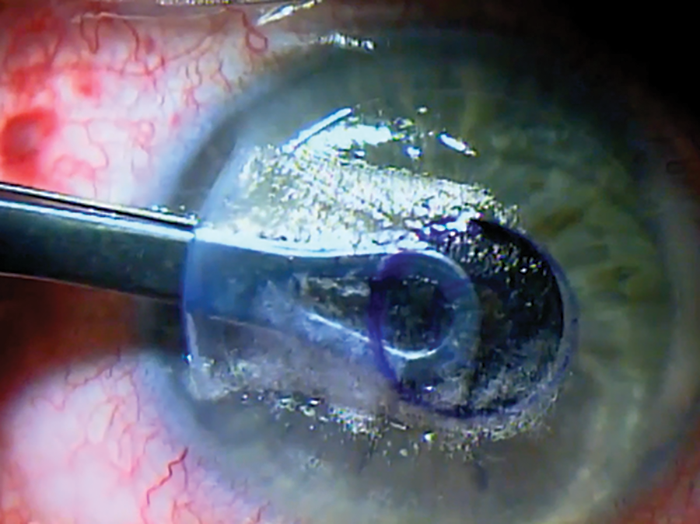
Figure 1. Dr. Wiley inserts the Kamra.
On postoperative day 1, the patient had a distance visual acuity of 20/20 in his dominant eye. Typically, my patients have a near visual acuity of 20/40 to 20/50 on day 1. By 1 to 3 months after surgery, they generally see 20/25 or better at near and 20/25 at distance.
SURGICAL TECHNIQUE
A Staged Approach
For surgeons new to inlay technology and/or the combined procedure, a staged approach is reasonable, while they become familiar with the technique. The inlay is placed 1 to 3 months after LASIK, once the nondominant eye has healed. In some cases, the patient may be satisfied with the results of laser correction and delay the inlay procedure until presbyopia progresses. The staged approach is also an option for pre-presbyopes (ie, patients who are approximately 40 years old). They benefit in the near term from mild monovision and undergo the inlay procedure later when it is needed.
With the staged approach, the surgeon creates a LASIK flap that is 80 to 100 µm thick in the nondominant eye. Later, during the second stage of the procedure, the inlay pocket should be made at least 100 µm below the LASIK flap to avoid intersection and at least 225 µm above the endothelium.
Same-Day Surgery
Performing LASIK and placing the corneal inlay on the same day is convenient for patients. At our practice, my colleagues and I have performed 200 of these procedures and have that found eyes tolerate it well.
I mark the cornea on the visual axis under a ring light. The patient is then moved under the femtosecond laser (iFS Laser; Johnson & Johnson Vision), and I create a tunnel that is 275 to 300 µm deep. I then make the LASIK flap 80 to 100 µm below the epithelium. After moving the patient under the excimer laser (Star S4 IR Excimer Laser system; Johnson & Johnson Vision), I use the ring light to guide my placement of the aperture inlay in alignment with the corneal mark. Using the HD Analyzer or the AcuTarget HD (both from Visiometrics), I confirm that the implant is well centered.
Next, I lift the flap, perform the ablation, reposition the flap, and place an extended-use punctal plug in the lower eyelid (Figure 2). The occlusion lasts approximately 3 months, and I find it ensures an adequate amount of tears on the ocular surface while the eye heals.
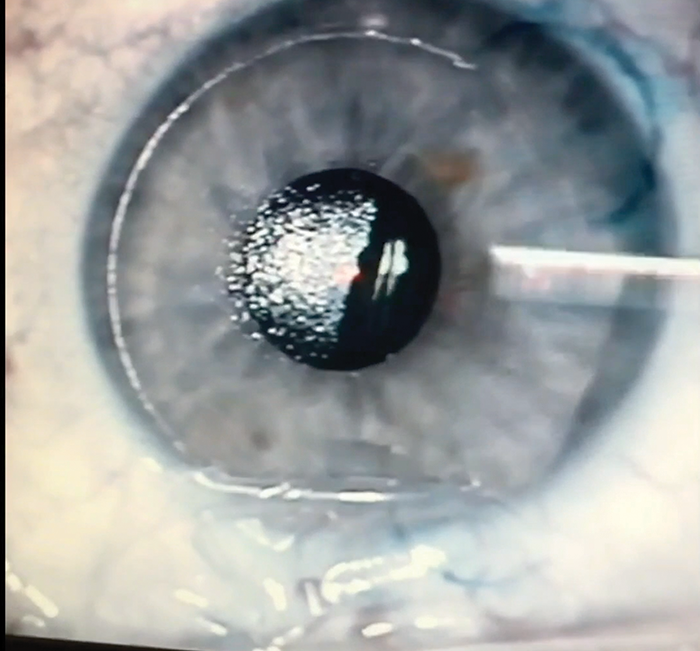
Figure 2. The Kamra is in place in the deep pocket, and the LASIK flap has been lifted back.