Keratoconus is the most common type of corneal ectasia.1 Classically, it is characterized by progressive corneal steepening and thinning that is asymmetrical between eyes; visual impairment eventually ensues due to increasing irregular astigmatism, higher-order aberrations, and/or corneal scarring.2
AT A GLANCE
- Patients with keratoconus may experience earlier onset of cataract-related visual symptoms, which may be confounded by their underlying ectatic condition.
- Early cataract evaluation, careful IOL selection and preoperative planning, and tailored surgical techniques are among the factors that help predict visual success.
- The magnitude of cataract surgeries performed worldwide demonstrates the safety of modern cataract surgical techniques.
Patients with subclinical or mild disease may not be binocularly symptomatic, leading to a delayed diagnosis or lack of one altogether. These patients are typically diagnosed later in life. A retrospective review reported that approximately 25% of patients with keratoconus are diagnosed after their fifth decade of life.3 It has also been reported that patients with keratoconus are at increased risk of developing cataracts at a younger age, with nuclear sclerosis being the most common manifestation.4 The same study found that the visual reductions in these patients were incorrectly attributed to corneal ectasia, highlighting the importance of earlier cataract evaluation in patients with keratoconus.
Below, we offer clinical pearls for managing patients with keratoconus and concurrent cataract.
SEPARATING CATARACT AND KERATOCONUS CONTRIBUTIONS
As an ectactic cornea becomes more stable with age, it may be puzzling to hear a patient with keratoconus complaining of worsening visual symptoms, especially if they are younger than the typical age of a cataract patient. In this scenario, a gas permeable (GP) lens refraction can help to determine if the source of the visual complaint is related to corneal changes (ie, significant symptom improvement with GP refraction) or lenticular changes (ie, limited improvement with GP refraction). The diagnosis of visually significant cataract can also be supported by serial tomography or topography imaging to confirm corneal stability. Additionally, densitometry grading of the crystalline lens captured during Pentacam tomography (Oculus) may be helpful.
CHALLENGES OF GRADING KERATOCONUS SEVERITY AND STABILITY
The determination of preoperative keratoconic stability and severity affects and complicates a surgeon’s IOL selection. There are multiple challenges in obtaining accurate preoperative biometric and keratometric data. For example, corneal steepening and distortion elevates the clinical complexities in estimating the true corneal power of keratoconic eyes.5 In terms of keratometry, some sources of errors include6,7:
- the instrument-measured keratometry often overestimates the corneal power because it does not coincide with the actual keratometry value at the visual axis of a keratoconic eye
- the anterior to posterior corneal radii ratio greatly varies among keratoconic corneas given the increasing posterior contribution, so the adapted corneal refractive index of 1.3375 in keratometric instruments has poor clinical application, and
- the irregular tear film commonly seen in keratoconic eyes reduces the repeatability of keratometry measurements.
Hashemi et al compared five devices and concluded that a Scheimpflug elevation-based tomographer provides the best measurement repeatability in keratoconic corneas with a maximum keratometry of ≤ 55.00 D.8 Therefore, a Scheimpflug tomographer could allow higher confidence in the clinical assessment of mild to moderate keratoconus patients during cataract evaluations.
GETTING PATIENTS READY FOR CATARACT EVALUATION
Given the clinical challenges, there are several factors to consider prior to cataract referral to help optimize surgical outcomes. Discontinuation of contact lens wear prior to cataract evaluation can better ascertain the relative accuracy in preoperative data of keratometry, topography, pachymetry, axial length, and manifest refraction. An acceptable contact lens holiday has been proposed as 2 weeks for soft lenses and 5 weeks for corneal GP lenses. Pending corneal stability, a longer discontinuation period may be needed. If keratoconus progression is demonstrated with serial imaging, patients may benefit from a UV light-mediated corneal stabilization procedure prior to cataract surgery.9 Additionally, ocular surface optimization can help minimize the negative effects of an irregular tear film and prevent a delay in surgical scheduling.
IOL CALCULATION
Apical decentration in keratoconus decreases the measurement reliability of both keratometry and axial length. Keratoconus has also been associated with higher myopia due to steeper corneal curvature, longer axial length, and deeper anterior chamber depth, all of which confound the ability of IOL formulas to predict the postoperative effective lens position, a key component in IOL power selection.10,11 These measurement errors overestimate the corneal power and lead to post-cataract hyperopic surprises. The effects of these errors become even more pronounced as keratoconic severity increases.
In anticipation of these biometric measurement errors, we suggest a few different approaches to facilitate IOL power calculations:
- use optical biometry devices to measure axial length and anterior chamber depth whenever possible,
- use newer-generation keratoconus-specific IOL formulas, such as the Kane keratoconus and Barrett True-K keratoconus formulas,
- compare across multiple formulas to crosscheck the suggested IOL power, and
- adjust input variables for the IOL formula (ie, keratometry and postoperative myopic targets) according to the disease severity of each patient with keratoconus.
Rather than entering the instrument-measured keratometric values into an IOL formula for patients with severe keratoconus with preoperative mean keratometry > 55.00 D, Watson et al suggested entering a standard value of 43.25 D instead.12 And when comparing nine IOL formulas in 147 patients with keratoconus, Kane et al showed that the Kane keratoconus formula yielded the most eyes (50%) within ±0.50 D across all severity stages.13 Moreover, to further reduce hyperopic surprises, Kane et al also recommended adjusting postoperative myopic targets to between -0.75 D and -1.50 D (in stage 2 from 48.00 D to 53.00 D), as well as between -2.00 D and -3.00 D (in stage 3 > 53.00 D).
IOL SELECTION
For most patients with keratoconus who return to contact lens wear after cataract surgery, we recommend monofocal IOLs to avoid the induction of residual astigmatism or other refractive aberrations. Some clinicians have considered IOLs with varying degrees of asphericity (often expressed as the Q value in an IOL) for both regular and irregular corneas. However, given that a keratoconic cornea is hyper-prolate with a large negative Q value, we recommend considering IOLs that are either neutral (Q = 0) or positive spheric (positive Q value), instead of aspheric.
In select cases, it may be possible to consider a toric IOL for a patient with stable keratoconus with good spectacle-corrected vision, low higher-order-aberrations, and low risk of future corneal transplant.14 Additionally, a capsular tension ring can be implanted with a toric IOL to prevent excessive postoperative IOL rotation.
CORNEAL INCISIONS AND WOUND CONSTRUCTION
When planning a corneal incision, the surgeon should account for the location of the corneal scar (if present), peripheral corneal steepening, and corneal thinning. An incision through a scarred area should be avoided because it will induce a higher and unpredictable amount of iatrogenic astigmatism. Additionally, peripheral incisions along locations of scar or extreme corneal steepening and thinning can increase the likelihood of wound leakage. If needed, a suture at the main incision site can be left intact for a few weeks to help with wound sealing. It is advised to create the main incision at a temporal location as near the limbus as possible (ie, a superotemporal incision in patients with an inferotemporal cone). Alternatively, a surgeon may choose to create a scleral tunnel incision with sutures to circumvent complications.14
RECOMMENDING A COMBINED CORNEAL PROCEDURE
Unavoidable measurement errors in patients with keratoconus generally result in hypermetropia and reduced patient satisfaction after cataract surgery. This underscores the potential benefit of recommending an additional corneal refractive procedure in select cases of patients with stable keratoconus to reduce disease severity before or during cataract surgery. The potential benefits of improved preoperative data accuracy and intraoperative ocular view can render enhanced outcomes for cataract surgery.
PATIENT EDUCATION AND POSTOPERATIVE MANAGEMENT
Patients with keratoconus may view cataract surgery as a way to improve UCVA and/or BCVA. Although this may be a possibility, as demonstrated in our patient case of combined corneal tissue addition keratoplasty (CTAK) and cataract extraction (Figures 1-3), clinicians should discuss management challenges with patients to set realistic postoperative goals. Patients should also understand that there may be a higher likelihood of requiring an IOL exchange or a secondary IOL.

Figure 1. Corneal tissue addition keratoplasty (CTAK). Femtosecond laser is used to create an intrastromal channel in the cornea (A). A gamma-irradiated corneal stromal insert is placed into the channel (B) and smoothed and rotated into position (C) until the stromal insert corresponds with the preoperative CTAK plan designed using tomographic data (D).

Figure 2. Before CTAK, Pentacam measurements and IOL calculations were made using the Kane keratoconus formula (A). Pentacam and IOL calculations 3 months after CTAK; note the improvement in irregular astigmatism and the significant change in monofocal IOL power of +7.00 D due to flattening of the central cornea (B).
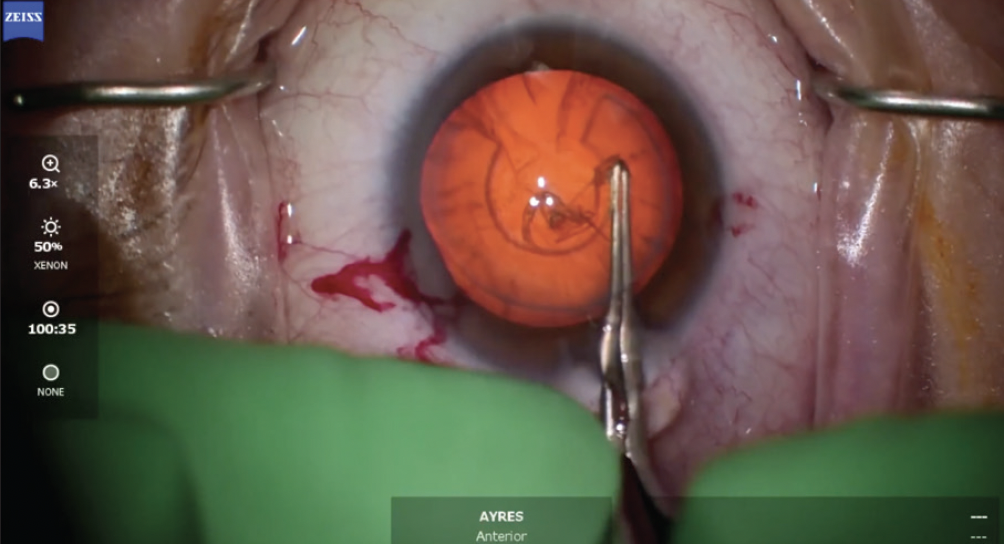
Figure 3. Surgical view through the CTAK segment in a patient with keratoconus undergoing cataract surgery after CTAK. The patient’s preoperative UCVA and BCVA were 20/200 and 20/70, respectively. Post-CTAK and cataract surgery, the patient’s UCVA and BCVA significantly improved to 20/70 and 20/30, respectively.
In a case series of 34 keratoconic eyes, Leccisottie et al reported IOL exchanges in 32% of study eyes due to unexpected refractive ammetropia.5 However, the need for IOL exchanges can be avoided if patients are scheduled to resume contact lens wear to achieve optimized postoperative visual outcomes. We recommend a minimal waiting period of 4 weeks before considering a return to contact lens use or a refit of the contact lens in the operated eye.
KNOW WHAT YOU’RE UP AGAINST
Patients with keratoconus may experience earlier onset of cataract-related visual symptoms, which may be confounded by their underlying ectatic condition. Thus, it’s important to recognize the benefits of early referral for cataract evaluation in keratoconus.
As far as we are aware, there has only been one case of keratoconic progression reported after cataract surgery.15 The magnitude of cataract surgeries performed worldwide demonstrates the safety of modern cataract surgical techniques. Nonetheless, it remains critical for all eye care providers to monitor their patients with keratoconus for corneal stability after cataract surgery.
1. Cronin B, Gunn D, Chang CY. Oxygen-supplemented and topography-guided epithelium-on corneal crosslinking with pulsed irradiation for progressive keratoconus. J Cataract Refract Surg. 2024;50(3):209-216.
2. Chang CY, Hersh PS. Corneal collagen cross-linking: a review of 1-year outcomes. Eye Contact Lens. 2014;40(6):345-352.
3. Yildiz EH, Diehl GF, Cohen EJ, Hammersmith KM, Laibson PR, Rapuano CJ. Demographics of patients older than 50 years with keratoconus. Eye Contact Lens. 2009;35(6):309-311.
4. Thebpatiphat N, Hammersmith KM, Rapuano CJ, Ayres BD, Cohen EJ. Cataract surgery in keratoconus. Eye Contact Lens. 2007;33(5):244-246.
5. Leccisotti A. Refractive lens exchange in keratoconus. J Cataract Refract Surg. 2006;32(5):742-746.
6. Gonzalez-Salinas R, Franco JJ, Reyes-Luis JL, et al. Cataract surgery in patients with underlying keratoconus: focused review. J Cataract Refract Surg. 2023;49(1):97-102.
7. Singh C, Joshi VP. Cataract surgery in keratoconus revisited – an update on preoperative and intraoperative considerations and postoperative outcomes. Semin Ophthalmol. 2023;38(1):57-64.
8. Hashemi H, Yekta A, Khabazkhoob M. Effect of keratoconus grades on repeatability of keratometry readings: comparison of 5 devices. J Cataract Refract Surg. 2015;41(5):1065-1072.
9. Spadea L, Salvatore S, Verboschi F, Vingolo EM. Corneal collagen cross-linking followed by phacoemulsification with IOL implantation for progressive keratoconus associated with high myopia and cataract. Int Ophthalmol. 2015;35(5):727-731.
10. Savini G, Abbate R, Hoffer KJ, et al. Intraocular lens power calculation in eyes with keratoconus. J Cataract Refract Surg. 2019;45(5):576-581.
11. Yağcı R, Güler E, Kulak AE, Erdoğan BD, Balcı M, Hepşen İF. Repeatability and reproducibility of a new optical biometer in normal and keratoconic eyes. J Cataract Refract Surg. 2015;41(1):171-177.
12. Watson MP, Anand S, Bhogal M, et al. Cataract surgery outcome in eyes with keratoconus. Br J Ophthalmol. 2014;98(3):361-364.
13. Kane JX, Connell B, Yip H, et al. Accuracy of intraocular lens power formulas modified for patients with keratoconus. Ophthalmology. 2020;127(8):1037-1042.
14. Moshirfar M, Walker BD, Birdsong OC. Cataract surgery in eyes with keratoconus: a review of the current literature. Curr Opin Ophthalmol. 2018;29(1):75-80.
15. Labiris G, Panagiotopoulou EK, Ntonti P, Taliantzis S. Corneal ectasia following cataract extraction surgery in a patient with keratoconus: a case report. J Med Case Rep. 2019;13(1):296.