The US Department of Veterans Affairs (VA) launched its Technology-Based Eye Care Services (TECS) in Atlanta in 2015. The goal was twofold:(1) to screen veterans for high-risk eye diseases where they receive primary medical care and (2) to improve their access to care. Four years later, this innovative, store-and-forward telemedicine program—in which patient information is collected at one point in time and care is delivered at a different point in time—is improving the overall health of an underserved patient population.
EYE CARE FOR VETERANS: OBSTACLES AND CONCERNS
Utilization surveys that the VA performs indicate that the VA’s patient population tends to be a lot older and to include a higher proportion of minorities compared with the general US population. The average age of veterans in the VA is 55 years compared with around 30 years in the general US population, and there are proportionally more Hispanic and black veterans. As such, veterans are more likely to have eye disease, yet their access to eye care can be problematic. In Georgia, for example, a large number of veterans live in rural communities far from an eye care provider. Moreover, a higher percentage of the homeless lives in rural areas, according to the US Department of Health and Human Services.
The increased prevalence of eye disease and difficulties accessing care (long travel distances, lack and/or cost of transportation)—especially among rural patients—create significant health care disparities in the general population and in veterans alike. Additionally, these barriers to access meant that many veterans living in Georgia were not presenting to an eye care provider until they had reached the late stages of various eye diseases. Obviously their prognoses would have been far better had these diseases been detected and treatment initiated earlier.
BEGINNINGS
My colleagues and I hypothesized that offering eye care closer to where veterans lived would improve access and as a corollary, we hoped, improve patient outcomes. To that end, we decided to test a telemedicine approach in partnership with primary care clinics. TECS started in three cities around Atlanta. The idea was to make it possible for veterans to have their eyes examined at the same time that they were having a routine well visit or attending a group session at a VA primary care clinic.
HOW THE PROGRAM WORKS
Patients can refer themselves, or they may be referred by their primary care physician at the VA. Patients with acute ocular issues or known eye disease are not eligible for TECS but are seen instead at one of the VA’s main eye clinics.
A specially trained certified ophthalmic technician is stationed full time at the primary care clinic in a VA medical center. This employee works out of a room measuring 120 square feet. He or she has access to trial lenses and a trial frame, an autorefractor, a lensometer, a tonometer, a nonmydriatic fundus camera, and a handheld pachymeter. Other equipment typically found in an exam lane is missing, such as a slit lamp and phoropter (Figure 1).

Figure 1. A TECS site in Atlanta.
The technician follows a detailed protocol for collecting information on each patient’s eyes. It begins with taking the patient’s history. Next, the technician determines the patient’s BCVA, measures IOP, and takes multiple photographs of the patient’s eyes with the nonmydriatic camera (Figure 2). All information is then uploaded to an electronic health record and reviewed by a physician who may be located miles away or in another state. This doctor reads the information, interprets the photographs, develops a medical assessment and plan, and prescribes glasses, if needed. Like the technician, the physician follows a protocol that specifies when patients should be referred for a subjective refraction or in-person examination.
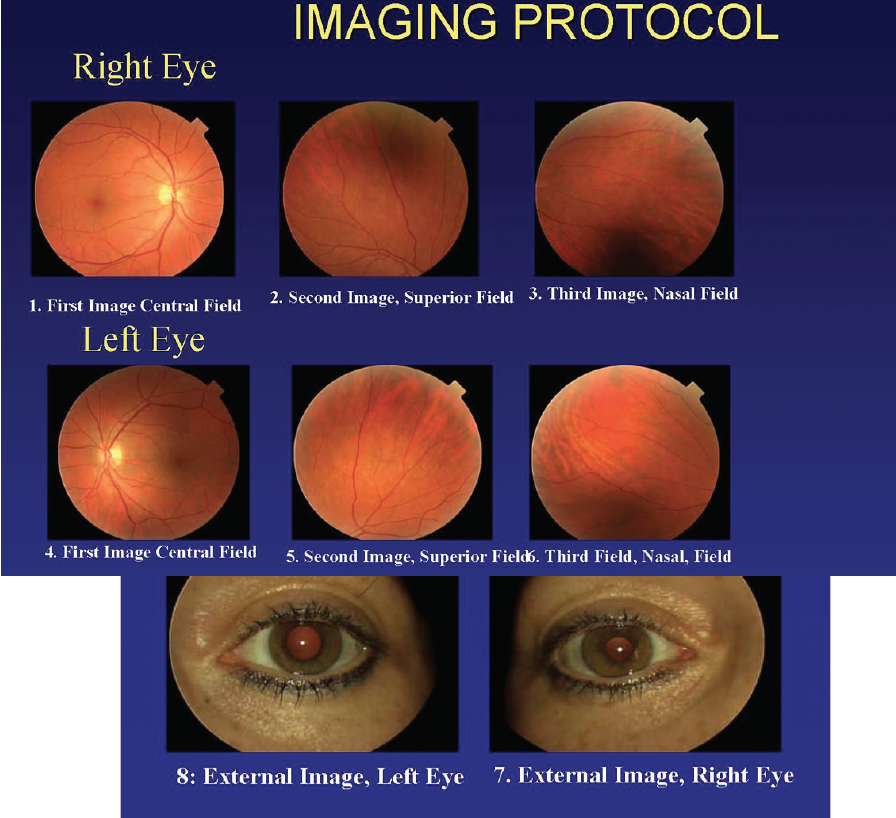
Figure 2. The TECS protocol calls for three 45º nonmydriatic photographs and one external photograph of each eye for every patient.
The VA provides free eyeglasses as a benefit to veterans. If a veteran participating in the TECS program requires glasses, the physician provides a prescription. The patient may then pick a frame style from a small display case in the TECS room and be fitted. The ophthalmic technician will measure pupillary distance and bifocal segment height and then order the glasses. If for some reason the patient does not like his or her glasses after receiving them, that will be logged into the system, and the glasses will be remade. The data are tracked so that we can compare our success with that of an eye clinic.
BENEFITS AND OUTCOMES
Based on the success of the Atlanta TECS sites,1 the TECS program has expanded nationally. We have a robust quality assurance/improvement system conducted by a third-party data team that measures several metrics. In terms of access to care, for example, we track appointment waiting times and no-show rates. Clinical care metrics include patient satisfaction, eyeglass remakes, reading consistency, image quality, disease detection (ie, how well diagnoses made in the TECS program match those made in person when a patient requires and attends a follow-up appointment), and length of visit.
Since its inception, the program has served approximately 18,000 patients. Patient satisfaction has been extremely high. The program has scored well on clinical convenience, service, and likelihood that a patient would recommend the program to another veteran.1
The greatest benefit that the TECS program offers is substantially improved access to eye care. More than 95% of veterans are generally able to obtain an eye screening within 30 days of requesting an appointment. Approximately half of them are seen on the same day as referral. When we initiated the program, approximately 8% of the veterans who used it had never been seen by an eye care provider in the VA. That number has dropped to about 5% because of the patients receiving eye care through the TECS program.
CHALLENGES AND OPPORTUNITIES
As noted earlier, the TECS program is not suitable for every patient. As with any telemedicine program, proper patient selection remains crucial to ensuring patient safety and high-quality service.
Follow-up care can also represent a challenge. When patients who access TECS receive a diagnosis that requires them to be seen face to face, it often means that they will have to travel farther to receive care, which can present barriers mentioned earlier (ie, cost and lack of transportation, extended travel time). The TECS program has a 30% referral rate, approximately 15% of which is for glaucoma and suspected glaucoma, 30% for cataract, 3.5% for age-related macular degeneration, 6% for diabetic retinopathy, and the rest for miscellaneous causes.
Another area we are looking to address is the range of testing capabilities offered at TECS sites. We are currently assessing whether it would be possible to include visual field testing and macular imaging through installation and use of a machine that combines fundus photography and OCT imaging, to permit what we call tele-follow-up for patients with mild disease and for low-risk glaucoma suspects.
CONCLUSION
Some providers may worry that telemedicine will replace them, but that has not been our experience. Rather, the TECS program has improved an underserved population’s access to eye care, reduced health care disparities, and maximized provider skill and time for the patients who need them the most.
Note: The views expressed in this article are solely those of the author and in no form represent the views of the federal government.
STATEMENT FROM THE AMERICAN OPTOMETRIC ASSOCIATION
As has been the case with most every aspect of Dr. April Maa’s flawed and continually shifting Technology-Based Eye Care Services pilot program (referred to as TECS), now under evaluation by Veterans Affairs health officials, this article represents yet another missed opportunity to address key questions about the program’s safety, efficacy, and costs. The American Optometric Association (AOA), which stands firm in safeguarding the recognized role of ODs as equal partners with ophthalmologists in providing the highest quality care to America’s veterans, has cited how the experimental TECS pilot threatens to mislead veterans and undermine the standard of care they need and deserve. National Veteran Service Organizations and concerned U.S. Senators and House members have weighed in as well, especially spotlighting the dangers connected to inadequate information, new cost burdens to veterans and the VA system, and the creation of barriers to essential primary eye care services. We urge Dr. Maa and those involved with her program to stop putting forward partial information and to start working with the AOA, veteran service groups, and Congressional leaders to do what’s right for veterans. For more information, please visit www. AOA.org or contact the AOA directly.
1. Maa AY, Wojciechowski B, Hunt KJ, et al. Early experience with technology-based eye care services (TECS): a novel ophthalmologic telemedicine initiative. Ophthalmology. 2017;124(4):539-546.