For patients undergoing cataract, refractive, or glaucoma surgery, failure to optimize the ocular surface before surgery may prevent favorable outcomes. It falls on optometrists to optimize the ocular surface before surgery and to know the nuances of ocular surface considerations for surgical patients.
CATARACT AND REFRACTIVE SURGERY
In our clinic, ocular surface evaluation is similar for cataract and refractive surgical patients. If the results of a dry eye questionnaire indicate ocular surface problems, our clinic staff obtains a full patient history, asking the patient about vision changes and common dry eye signs and symptoms. We use this information as a starting point to initiate diagnostic testing (Figure 1).
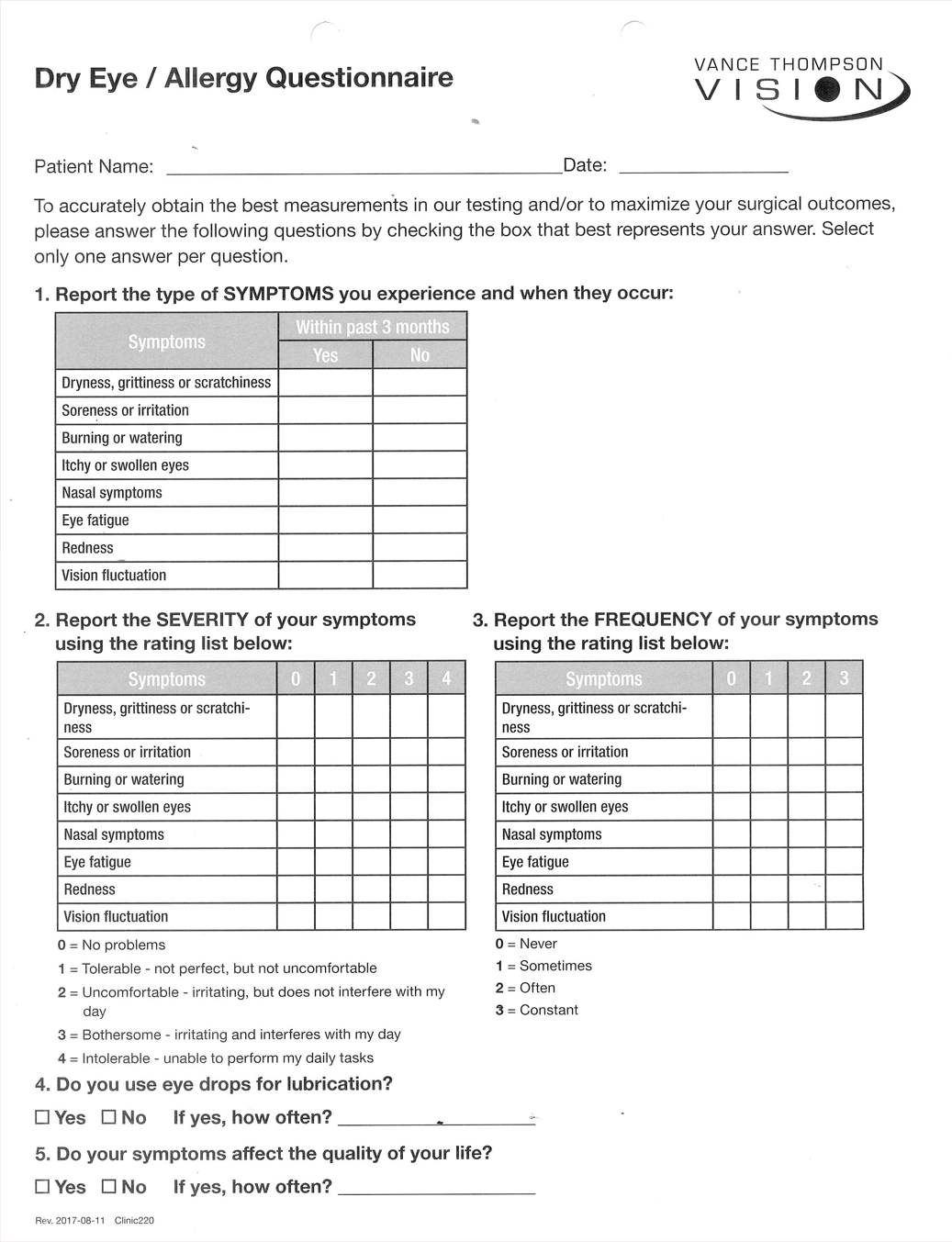
Figure 1. The modified SPEED questionnaire used at Vance Thompson Vision. The results of this questionnaire guide the clinic toward appropriate diagnostic testing.
For all positive questionnaires, our clinic performs tear osmolarity testing using the TearLab Osmolarity System (TearLab). We emphasize identification of meibomian gland dysfunction (MGD), which can change the patient’s refractive measurements, topography measurements, biometry measurements, and may cause dry eye.1 Meibum that is thin and oily indicates healthy meibomian gland function, whereas toothpaste-like expression indicates that a gland is likely impacted and will require intervention. We perform meibography using either LipiScan (Johnson & Johnson Vision) or LipiView (Johnson & Johnson Vision) in patients with suspected impacted meibomian glands (Figure 2). Other meibography options include the Meibox (Box Medical Solutions) and the Meibo-scan function on the Keratograph 5M (Oculus).
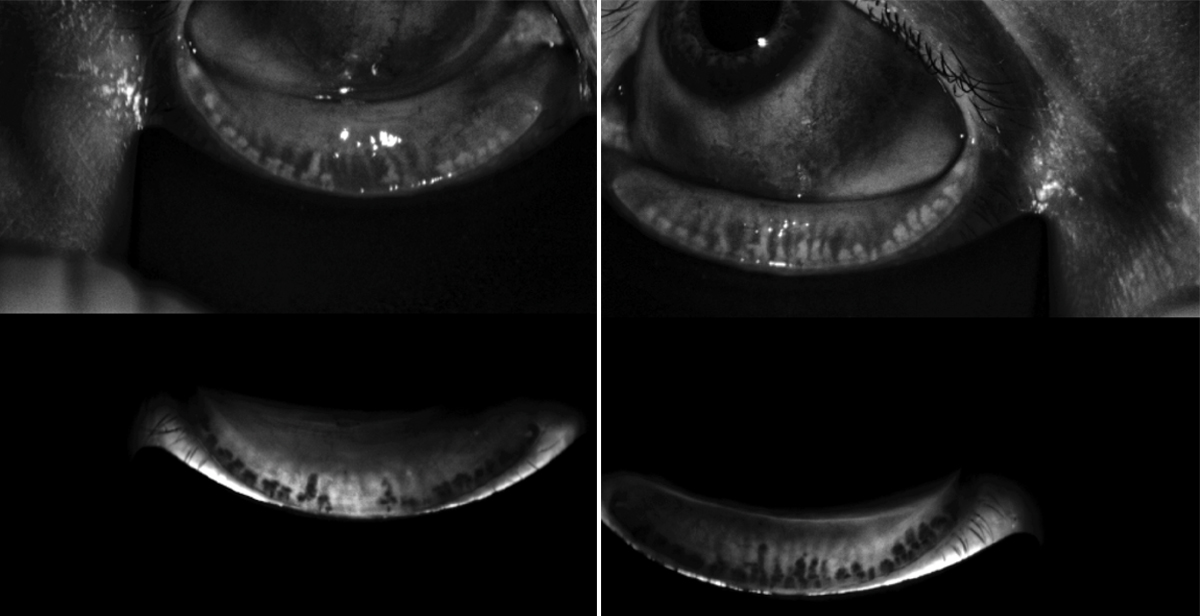
Figure 2. A meibography image of a patient with advanced MGD and gland atrophy.
We also measure tear breakup time in dry eye suspects using the Ocular Scatter Index on the HD Analyzer (Visiometrics). This documentation of light scatter at the refractive surface is valuable for planning surgery and educating patients about dry eye.
In patients with abnormal tear osmolarity or corneal staining, decreased tear breakup time, and complaints of symptoms consistent with ocular surface disease (OSD), we initiate treatment with either cyclosporine ophthalmic emulsion 0.05% (Restasis, Allergan) or lifitegrast ophthalmic solution 5% (Xiidra, Shire). Treatment also may include ocular steroids, punctal plugs, and lid hygiene regimens. For patients with MGD, we may perform vectored thermal pulsation with LipiFlow (Johnson & Johnson Vision) to clear obstructions and help restore healthy function. Other platforms that rely on heat to clear obstructed meibomian glands include the forthcoming TearCare platform (Sight Sciences) and the recently released iLux device (Tear Film Innovations).
With these treatments at our disposal, we can generally optimize the ocular surface for surgery without a significant delay. However, in certain cases where OSD is negatively affecting topography or biometry measurements, surgery may need to be delayed until treatment is initiated.
GLAUCOMA SURGERY
Many patients with glaucoma use topical medications, and 66% of patients using glaucoma drops have OSD.2 The primary reason glaucoma surgery is performed is to persevere vision and lower IOP, but the ocular surface should not be ignored in this patient population.
It is ideal to avoid adding more drops to a glaucoma patient’s already complicated topical medication routine before surgery. If MGD is present, vectored thermal pulsation may adequately address the condition. Alternatively, the TrueTear neurostimulation device (Allergan) can be considered. The device is inserted into the nasal cavity to stimulate the trigeminal nerve, which regulates the lacrimal tear system. Over time, the induced physiologic tear response may help prepare the ocular surface for surgery.
By helping to control IOP, traditional glaucoma procedures and microinvasive glaucoma surgery may reduce postoperative medication use, thus reducing toxicity and alleviating OSD. Patients should be reevaluated for OSD if a drop regimen is reduced or eliminated after surgery.
THE OD’S PRESURGICAL ROLE
Planning is key in all aspects of medicine, and eye care is no exception. Optometry’s role in the surgical spectrum of care straddles the surgery itself, and without proper preoperative preparation, the postoperative period may be beset with complications.
- Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15(3):438-510.
- Saini M, Vanathi M, Dada T, et al. Ocular surface evaluation in eyes with chronic glaucoma on long term topical antiglaucoma therapy. Int J Ophthalmol. 2017;10(6):931-938.






