Glaucoma is the leading cause of irreversible blindness worldwide.1 Given its increasing prevalence, optometrists have been taking a larger role in glaucoma management. OCT and automated perimetry are two of our most important tools, as they can quickly and reproducibly assess the structure and function, respectively, of the optic nerve and ultimately guide treatment.
AUTOMATED PERIMETRY
Visual field (VF) testing has long been the gold standard for the diagnosis of glaucoma and evaluation of its progression. Automated perimetry units provide fast, repeatable tests with reliability factors assessed throughout testing to help the examiner gauge the test’s quality. Printouts from the automated perimeter can provide both numerical and deviation maps of the patient’s VF and indices such as VF index, mean deviation, and pattern standard deviation that can be used to track glaucoma progression over time. These automated measurements allow comparison of test results over time via progression analysis, a program in the VF software that helps evaluate specific points of change or progression on deviation plots. VF indices can be plotted over time to evaluate trends in glaucomatous damage.
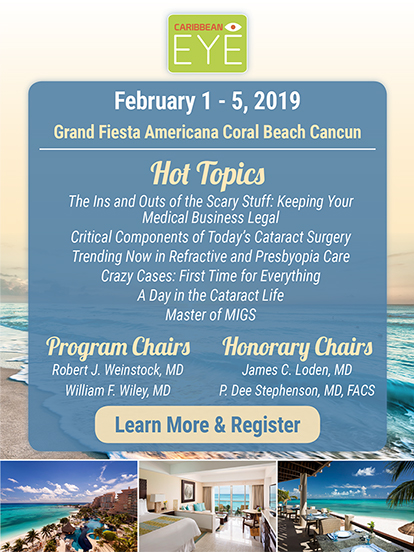
A variety of testing patterns can be used to assess various areas of the VF. For patients with early-stage glaucoma, wide field testing such as the 24-2 protocol on the Humphrey Visual Field Analyzer (Carl Zeiss Meditec) are commonly used to detect early symptoms such as nasal step and arcuate defects (Figure 1).2 More concentrated central visual field testing, such as the 10-2 protocol on the Humphrey device, can be used in patients with advanced glaucoma when the field has already significantly constricted. Recent trends suggest the utility of using the 10-2 test in earlier disease stages, as low sampling of the central VF in the 24-2 protocol may miss progression of macular damage.3
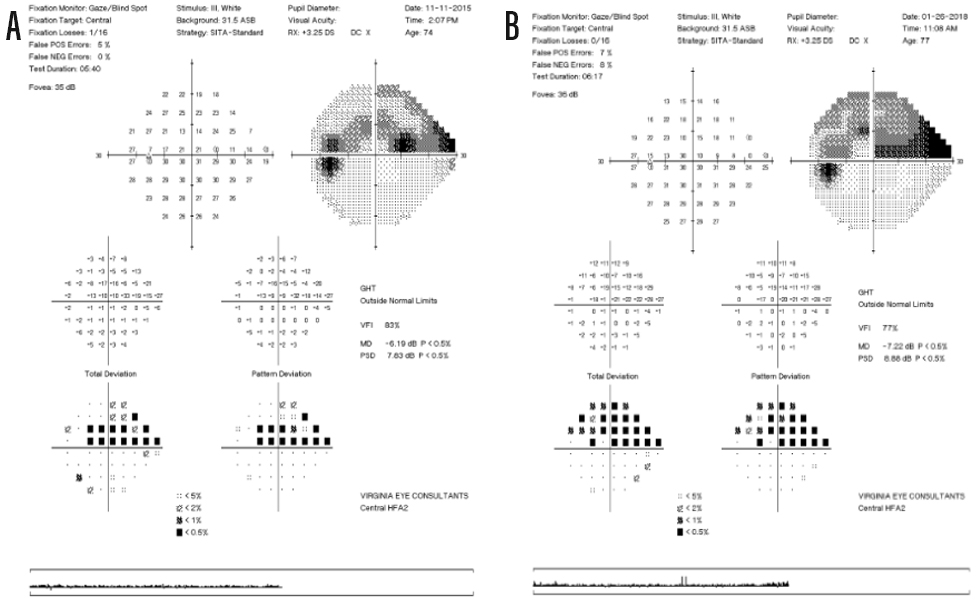
Figure 1. Standard printouts of 24-2 visual field tests in 2015 (A) and 2018 (B). Note the increased defect density on the deviation and grayscale plots. The indices on the right hand side in each printout also indicate progression (VFI, VF index; MD, mean deviation; PSD, pattern standard deviation).
Each test should be evaluated for validity, as there is a significant subjective component involved in VF testing. Any new VF defects should be compared with OCT findings and the appearance of the optic nerve on fundoscopy to determine the extent of glaucomatous damage or change.
OCT
Structural changes may precede or coincide with VF defects. OCT is a valuable tool for evaluating changes to the retinal nerve fiber layer (RNFL) and macular ganglion cell–inner plexiform layer (GC-IPL), showing subtle damage and changes that would be nearly impossible to see on fundoscopy alone (Figure 2).
Figure 2. Spectralis OCT (Heidelberg Engineering) scans of the patient in Figure 1. Note the dense defects in the inferotemporal area of the retinal nerve fiber layer scans in both eyes (A) and the corresponding loss inferiorly on the ganglion cell–inner plexiform layer scan (B). These defects directly correspond with the dense visual field defect seen in the left eye in Figure 1.
Like automated perimetry, OCT platforms integrate progression analysis to allow tracking of changes over a series of tests. OCT is especially useful in imaging patients with early-stage glaucoma, as changes may be seen on consecutive OCT tests before any defects manifest on VF testing, leading to earlier diagnosis of glaucoma.4
At later stages of glaucoma, evaluation of the RNFL will show a floor effect, which means that the RNFL has been depleted to such a level that factors such as glial cells and blood vessels limit the amount of “thinning” that can be observed on OCT. When the floor effect occurs, evaluation of the GC-IPL may still be sensitive to changes and should be carefully studied.5,6 VF testing also begins to take on greater importance at these severe stages of disease.
HARMONIOUS USE IS KEY
The ability of automated perimetry and OCT to provide trackable data to evaluate functional and structural changes over time make these platforms essential tools in glaucoma management. Although neither test is foolproof on its own, proper use of these technologies together allows eye care providers to treat patients appropriately and decrease the likelihood of future vision loss.
- Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262-267.
- Khoury J, Donahue S, Lavin P, Tsai J. Comparison of 24-2 and 30-2 perimetry in glaucomatous and nonglaucomatous optic neuropathies. J Neuroophthalmol. 1999;19(2):100-108.
- Grillo LM, Wang DL, Ramachandran R, et al. The 24-2 visual field test misses central macular damage confirmed by the 10-2 visual field test and optical coherence tomography. Transl Vis Sci Tech. 2016;5(2):15.
- Kuang T, Zhang C, Zangwill LM, et al. Estimating the lead time gained by optical coherence tomography in detecting glaucoma before development of visual field defects. Ophthalmology. 2015;122(10):2002-2009.
- Bowd C, Zangwill LM, Weinreb RN, et al. Estimating OCT structural measurement floors to improve detection of progression in advanced glaucoma. Am J Ophthalmol. 2017;175:37-44.
- Belghith A, Medeiros FA, Bowd C, et al. Structural change can be detected in advanced-glaucoma eyes. Invest Ophthalmol Vis Sci. 2016;57(9):OCT511-OCT518.