Unexplained spontaneous vitreous hemorrhage (VH) may result from myriad conditions, including ischemic retinopathy, Valsalva retinopathy, retinal artery macroaneurysm, retinal tear, and retinal detachment. In some cases, retinal imaging may detect subtle retinal changes that indicate the need for urgent care.
CASE PRESENTATION
A 69-year-old Hispanic woman was referred for evaluation of VH with corresponding decreased vision OS 3 weeks prior. The patient reported that her vision had improved since the time of referral and that she saw floaters in the affected eye, but she denied seeing flashes of light OS. She also reported no history of trauma, systemic disease (such as diabetes), or use of medication (such as anticoagulants).
Her BCVA was 20/20 OD and 20/25 OS. There was no evidence of neovascularization. Dilated examination revealed normal findings OD, and a resolving dehemoglobinized hemorrhage in the inferior vitreous was noted OS. A suspicious peripheral retinal vessel with scattered intraretinal hemorrhages in the inferonasal retina was also noted (Figure 1).

Figure 1. Fundus photo OS shows suspicious retinal vessel (red box) and scatted intraretinal hemorrhages in the inferonasal retina.
High-definition spectral-domain OCT (SD-OCT) revealed a partial posterior vitreous detachment (PVD) and traction on a vessel leading to the vitreous hemorrhage and a small retinal break (Figure 2). A shallow neurosensory detachment was also noted on imaging (Figure 3).
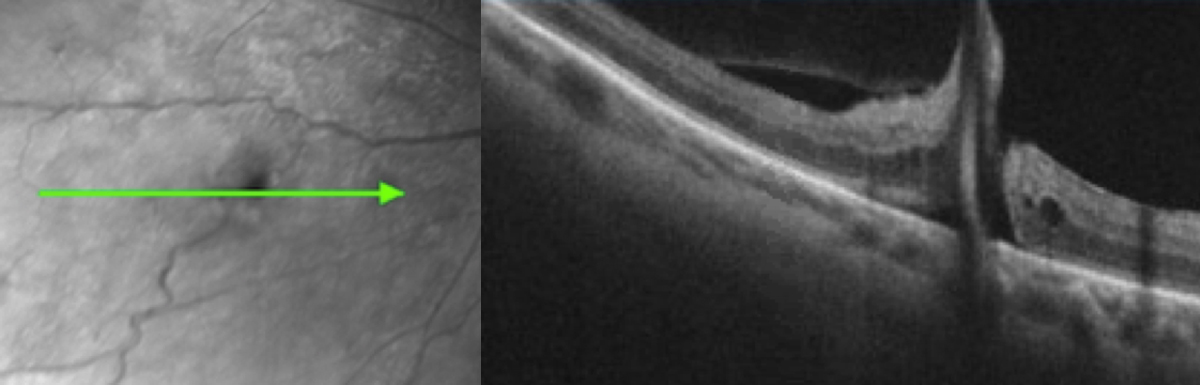
Figure 2: High-definition spectral-domain OCT OS showed an isolated full-thickness retinal defect with partial posterior vitreous detachment.
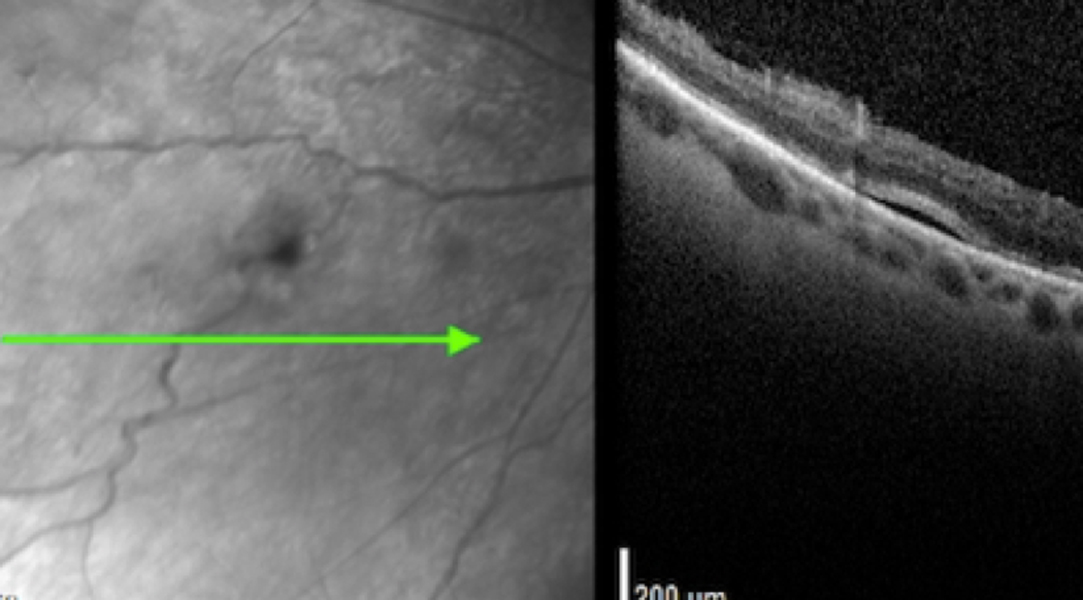
Figure 3: High-definition spectral-domain OCT OS revealed an isolated shallow area of fluid adjacent to the retinal break.
TREATMENT
A cause of VH may be attributed to a partial PVD that results in a torn or avulsed retinal vessel. VH can occur without sequelae in a small percentage of cases (<10%) as a result of a complete PVD, but when a hemorrhagic PVD occurs the risk of an underlying retinal tear increases to nearly 70%.1,2
This case represented a diagnostic challenge. The patient’s spontaneous VH was likely caused by a partial PVD with persistent traction leading to a torn retinal vessel. High-definition SD-OCT revealed an isolated retinal tear with shallow neurosensory detachment in the midperipheral nasal retina. She was referred for urgent evaluation and treated with laser photocoagulation.
Spontaneous unexplained VH represents a high risk for retinal tears or detachment. Advanced imaging techniques can enhance our ability to detect subtle retinal tears or defects that may be missed on ultrasound. Early detection and urgent management are invaluable in preventing vision loss or complications.
- Sarrafizadeh R,Hassan TS, Ruby AJ. Incidence of retinal detachment and visual outcome in eyes presenting with posterior vitreous separation and dense fundus-obscuring vitreous hemorrhage. Ophthalmology. 2001;108:2273-2278.
- SaxenaS, Jalali S, Verma L, Pathengay A. Management of vitreous hemorrhage. Indian J Ophthalmol. 2003;51:189-196.