Scleral lenses have become a widely used treatment modality for patients with corneal irregularity or corneal surface dryness. For many of these patients, the immediate benefits of wearing a scleral lens outweigh the potential long term complications of scleral lens wear. However, practitioners need to understand how scleral lenses can interact with the structure of the anterior segment in order to avoid compromising an already challenged eye.
It has been suggested that scleral lens wear may potentially lead to increased intraocular pressure (IOP).1 Because small-diameter lenses rest on the conjunctiva closest to the limbus and directly over drainage structures of the eye, they may be more likely to cause an elevation of IOP compared with larger-diameter scleral lenses. Scleral lenses are known to settle with wear time, and the effect of this settling on underlying eye structures is unknown. Could scleral lenses put enough pressure onto the episcleral veins and aqueous humor drainage sites to compromise aqueous humor outflow, resulting in increased IOP?
BETWEEN-EYES STUDY
To help shed some light on this issue we conducted a study in which IOP changes were measured in normal eyes with short-term small-diameter scleral lens wear. The study was approved by the Mayo Clinic’s institutional review board (IRB) and adhered to the tenets of the Declaration of Helsinki. All those recruited agreed to participation in the study before any measurements were made.
Twenty-nine individuals with no history of scleral lens wear and no ocular disease were recruited for the study. Mean age was 29 ± 6 (standard deviation) years; 19 patients were female and were 10 male. These patients wore a 15.0 mm Jupiter scleral lens (Visionary Optics) for 2 hours in one randomly chosen eye. The fellow eye served as a control, with no lens wear.
Lenses from a standard fitting set were selected to give 200 to 300 µm clearance centrally after the lens was placed. No corrections were made to improve vision or to optimize haptic alignment. After the appropriate study lens was selected for each participant, that person then returned on a different day to complete IOP measurements with lens wear.
On the day of the study visit, participants were asked not to wear any lenses prior to testing. (Seventeen of the participants were current soft lens wearers). Before lens placement, central and peripheral (2 mm temporal from the limbus) IOP measurements were made with pneumotonometry (»Model 30 Classic; Reichert) on both the study and control eyes. While the lens was in place, peripheral measurements only were obtained on the study eye at 5, 60, and 120 minutes after lens application, and both peripheral and central measurements were obtained at 5, 60, and 120 minutes in the control eye. Central measurements were obtained for the study eye immediately after lens removal.
RESULTS
Before the lens was placed on the study eye, mean IOP in the control eyes was 13.7 ± 2.2 mm Hg centrally and 18.4 ± 3.2 mm Hg peripherally. Mean IOP in the study eyes was 13.6 ± 1.9 mm Hg centrally and 18.4 ± 3.0 mm Hg peripherally. Central measurements were not different between eyes (P = 0.08; paired t-test), and peripheral measurements were not different between eyes (P = .9). Peripheral measurements were higher than central measurements in both study and control eyes (P < .001).
Within 5 minutes of scleral lens placement, mean peripheral IOP in the study eyes was 17.6 ± 3.9 mm Hg, and mean IOP in the control eye was 18.3 ± 3.4 mm Hg; this difference was not statistically significant (P = .3; Figure). No difference was noted in mean peripheral IOP between study eyes (18.4 ± 4.5 mm Hg) and control eyes (18.0 ± 3.4 mm Hg; P = .2) after 1 hour of lens wear. After 2 hours of lens wear, there was still no difference in mean peripheral IOP between study eyes (18.7 ± 3.9 mm Hg) and control eyes (18.1 ± 3.1 mm Hg; P = .2).
After 2 hours, immediately after lens removal, mean central IOP was not different between control eyes (13.5 ± 2.2 mm Hg) and study eyes (13.9 ± 3.1 mm Hg; P = .4). After 2 hours of lens wear, mean central IOP in the study eyes was not different from mean central IOP in the study eyes prior to lens wear (P = .6).
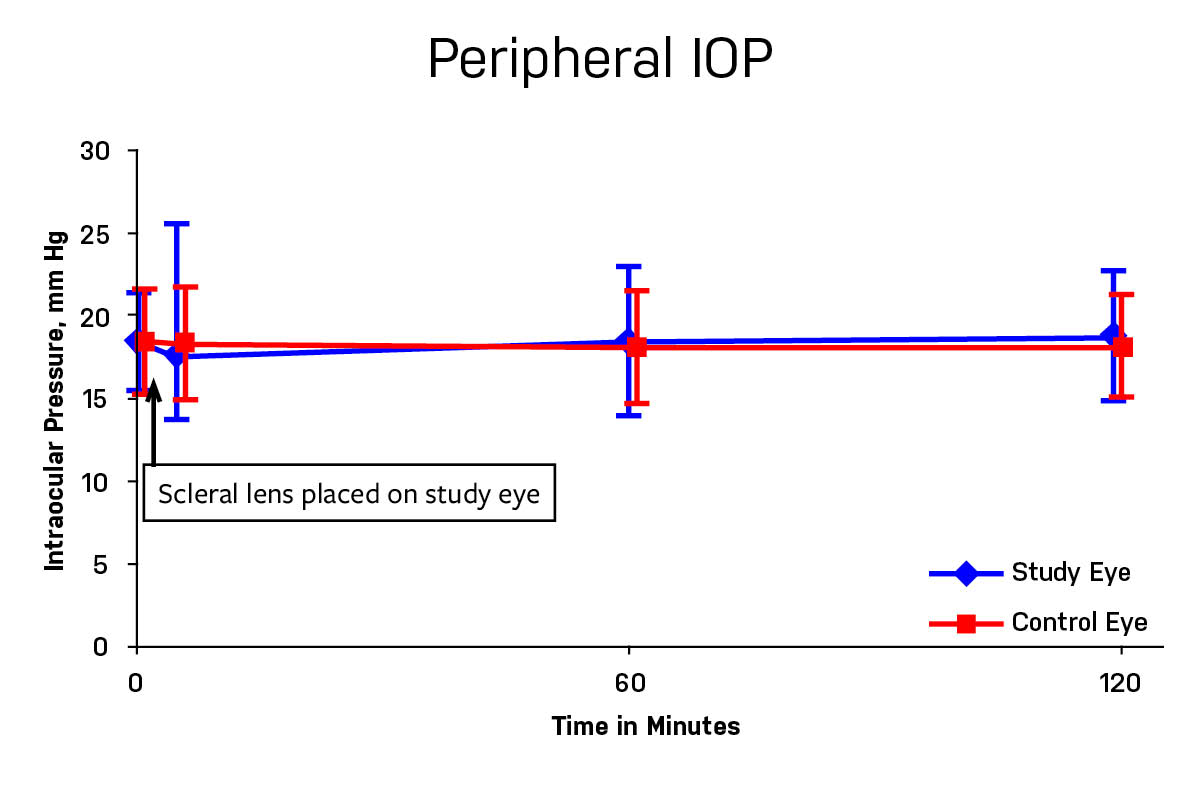
Figure. Peripheral IOP measured in the control eye (red square) and the study eye with the scleral lens (blue diamond). There was no significant difference between eyes prior to lens wear, or any time measured after lens wear.
CONCLUSIONS
As detailed above, no difference was detected in IOP between control eyes and eyes wearing a small diameter scleral lens for 2 hours. Assumptions that can be made from this study are limited by several factors. First, only young, healthy eyes were measured; aged or diseased eyes may have responded differently. Second, with longer wear times or more habitual wear, IOP findings might also be different.
It is promising that no early changes in IOP were found with short term scleral lens wear, but more study is needed before we can safely conclude that scleral lens wear does not affect IOP.
- McMonnies CW. A hypothesis that scleral contact lenses could elevate intraocular pressure. Clin Exp Optom. 2016;99(6):594-596.








