Keratoconus is a progressive condition characterized by central thinning and inferior steepening of the cornea. The condition is easy to miss during a conventional eye exam. The slit-lamp exam does not allow us to diagnose early keratoconus because the cornea will appear normal until there are significant corneal shape changes. Even patients with mild to moderate keratoconus, who have lost BCVA, can have a normal appearing cornea on slit-lamp examination.
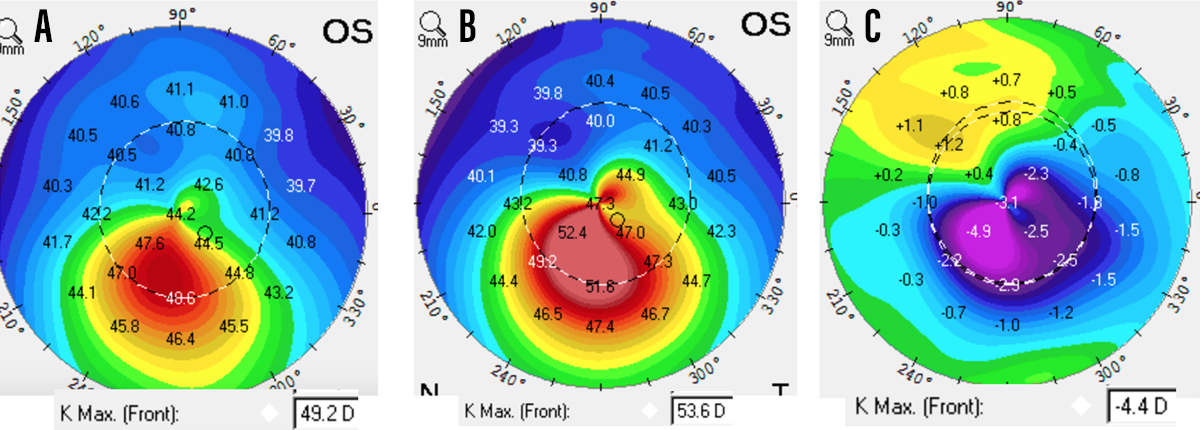
Corneal mapping with topography or tomography is necessary to effectively diagnose this condition (Figure 1). Patients who are experiencing changes in their refraction, especially the development of myopic astigmatism, are at increased risk for having keratoconus. We can gauge the severity of keratoconus by evaluating corneal shape and BCVA. With worsening keratoconus, there will be a loss of BCVA, and the corneal shape will demonstrate progressive steepening and advancing astigmatism.
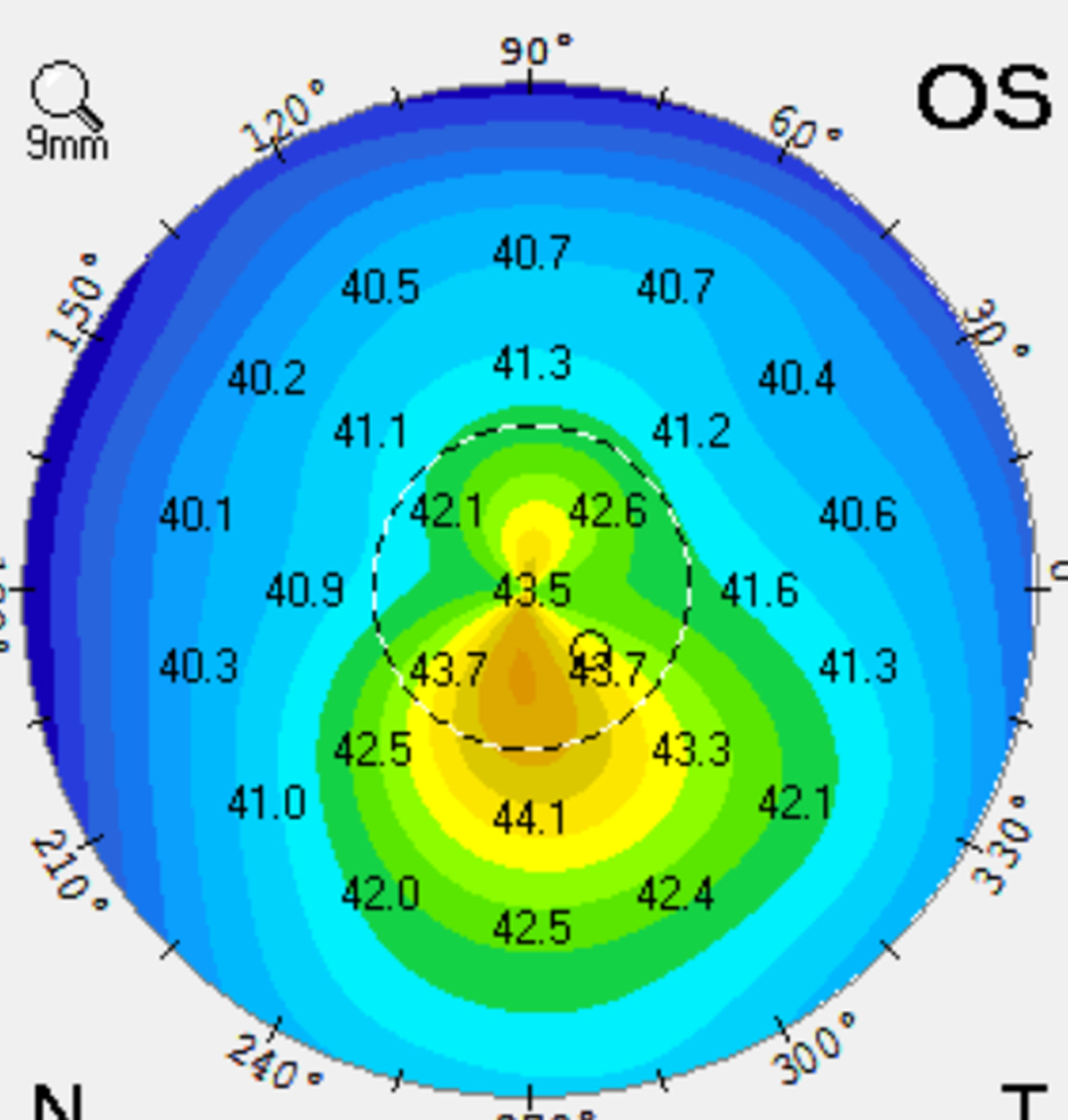
Figure 1. Corneal map of an eye with early keratoconus.
For example, if a patient who starts off with -3.00 D of myopia with 1.50 D of astigmatism, and returns the following year with 0.50 D of additional myopia, as well as an additional 0.75 D of astigmatism, one should be suspicious that early keratoconus may be present. Because not all practices have a topographer, one can refer that patient to a practice with the appropriate technology to evaluate corneal changes. If findings consistent with keratoconus are found, which could include central thinning, inferior steepening on corneal topography, and asymmetry between the two corneas, the patient may be referred for corneal collagen crosslinking (CXL).
Keratoconus does not discriminate: It is more common in younger patients, but older patients can develop keratoconus as well. That said, keratoconus can progress rapidly during childhood and adolescence, so careful monitoring at these ages is key. If keratoconus goes undiagnosed, the condition worsens and can result in significant vision loss. The sooner patients are identified and treated, or referred for treatment, the better.
TREATMENT OPTIONS
The prognosis for keratoconus, if treated, is excellent. There are two main goals for treatment. The first goal is to stop the progression of the disease with CXL. The second goal is to improve vision with technologies that include glasses and soft contact lenses in mild cases, and scleral contact lenses in patients who have experienced a reduction in BCVA. Other treatments that have the potential to improve vision include Intacs (AJL Ophthalmic) as well as topography-guided PRK.
Most patients who have keratoconus are candidates for CXL; the procedure can stabilize the condition and prevent progression. The CXL procedure can improve the corneal shape, and can also improve both uncorrected VA and BCVA. We therefore perform CXL in patients with all levels of keratoconus, although patients with mild corneal changes and crisp corrected vision can be observed.
Scleral contact lenses are also an option for patients with keratoconus, especially when there is a loss of BCVA with spectacles. This lens technology vaults over the cornea, and can dramatically improve a patient’s vision for the duration of time that the device is worn.
In some cases, either CXL or scleral lenses are sufficient independent of each other. In other cases, the two go hand in hand. For instance, if a patient who has keratoconus is seeing well with spectacles, one might opt to perform CXL and have the patient continue wearing glasses. In other instances where patients have inadequate vision with spectacles, the choice might be to perform CXL and then fit the patient for scleral lenses to improve vision further.
If keratoconus has progressed to the point where a patient cannot see well enough to function independently, he or she may benefit from scleral lenses fitting before undergoing CXL. The risk of this scenario is that the refractive error and vision may change rapidly, making the recently prescribed scleral lenses off-target. However, in our experience, the rate of change in vision after CXL is slow, and the same scleral lenses will typically work well for patients even a year after CXL.
SCIENCE FOR THE WIN!
Innovations such as CXL allow eye care providers to help patients whose condition was previously responsive to therapy, or whose condition was never addressed. It is another example of how eye care is one of the most exciting disciplines in medicine thanks to the constant innovation in the field.