

Mechanical dry eye (MDE) is one of the most common age-related eye diseases. In a study of approximately 1,500 participants older than 60 years, more than 98% demonstrated signs of MDE.1 Our practice is home to a dedicated dry eye clinic where MDE is routinely diagnosed and treated.
MDE is commonly known as conjunctivochalasis (CCh). However, there has been a steady, specialty-wide shift toward using the term MDE instead of CCh. We prefer MDE because it better describes the clinical condition. That is, CCh is an anatomic finding that may or may not cause clinical compromise. MDE refers to the condition that develops due to CCh, characterized by redundant folds of conjunctiva visible at the lid margin that often create a foreign body sensation, obstruct the punctum, and obliterate the normal tear reservoir and meniscus.
AT A GLANCE
- Mechanical dry eye (MDE) is a term that is coming into favor in lieu of conjunctivochalasis because the former term better describes the clinical condition.
- The redundant conjunctival tissue in MDE occupies the tear reservoir and prevents the eye from holding tears, causing pain and irritation.
- An outpatient procedure known as reservoir restoration can help to relieve symptoms in many patients with MDE.
PATHOLOGY
MDE is often thought of as a disease of the conjunctiva, but this is a misnomer because it is, in fact, degeneration of Tenon capsule due to chronic inflammation from matrix metalloproteinases (MMPs). A look at MDE pathology illustrates that Tenon capsule becomes a fibrovascular gel that can no longer support the conjunctival tissue. This process leads to shortening of the fornix with resultant loose, redundant conjunctiva visible at the lid margin (Figure 1). This degenerated loose tissue occupies the tear reservoir and prevents the eye from holding tears, and it may cause pain and irritation that feels similar to dry eye symptoms. Additionally, MDE may cause excessive tearing due to obliteration of the tear reservoir and/or obstruction of the puncta. Eye pain may be significant in patients with MDE, especially when they are blinking or gazing down. In most patients with MDE, pain is worse in the morning upon waking.2
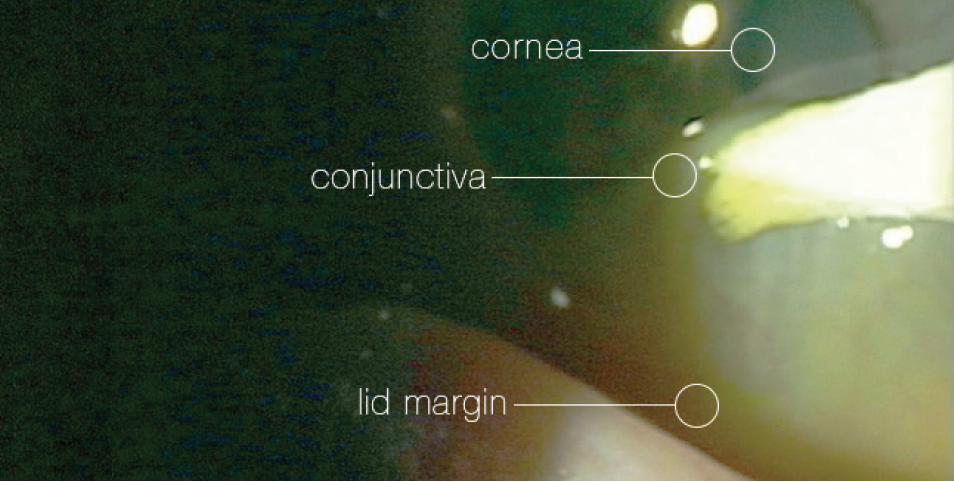
Figure 1. Surgical sponge lifting the separated conjunctiva partway up the cornea, demonstrating degree of MDE.
Photo courtesy of Douglas K. Devries, OD.
TREATMENT
MDE often occurs in combination with other forms of ocular surface disease (OSD), namely aqueous tear deficiency, blepharitis, and ocular allergies.3 Some cases of MDE are mild and sufficiently controlled with tear substitutes, lubricants, corticosteroids, or antihistamines. In other instances, patients may not respond to medical treatment, and these individuals are candidates for an outpatient surgical procedure that we call reservoir restoration, in which cryopreserved amniotic membrane is used to deepen the tear lake and restore the patient’s ocular anatomy to its normal state.
Optometrists are best suited to diagnose and initiate therapy for MDE. Given the prevalence of the condition, we discuss it early in our consultations with every dry eye patient. Patients who have MDE can be very frustrated; the condition is often misdiagnosed or overlooked because its symptoms are similar to those of other types of OSD.3 When we see that a patient does not respond to artificial tears and other topical therapeutics, we know it is appropriate to move forward with a more targeted discussion about MDE and its treatment.
We have found that there are three groups of patients with MDE: those who are asymptomatic; those who have symptoms but are controlled with conventional topical therapy or are living with the discomfort; and those who are symptomatic and extremely uncomfortable despite topical therapy. This latter group typically includes the patients who are searching for answers and are open to surgical options to control their condition.
COMANAGEMENT
An important part of working in tandem to diagnose and treat patients with MDE is that we each have a different conversation with the patient based on our areas of expertise. These two perspectives ultimately provide the full body of knowledge the patient needs to make a decision about whether to opt for surgery. Our aim is to be sure that the patient has already expressed interest in the procedure by the time he or she is referred for surgery.
Surgical treatment of MDE should happen in conjunction with topical therapy, not typically as a standalone treatment. An inadequate response to traditional topical therapy with tears and prescription medications is one sign that MDE may be a significant factor in OSD, which helps us to identify patients most likely to benefit from surgery. As previously mentioned, these are also generally the patients who are most highly motivated to proceed to surgical treatment.
When we describe the reservoir restoration procedure, we explain that we are restoring the normal anatomy of the ocular surface to help the patient better respond to topical therapy. We are careful to make sure the patient understands that we are treating a chronic condition, and therefore comanagement is important because the patient will need continuing therapy.
For optometrists who are interested in comanaging this condition, we recommend working with a surgeon who will address the full underlying pathophysiology, not merely resect the visible redundant conjunctiva or, worse yet, dismiss the role of MDE in OSD.
SURGERY AND AMNIOTIC TISSUE
Reservoir restoration is a minor surgical procedure that is performed under topical anesthesia. Designed to reestablish the normal anatomic tear reservoir in the inferior conjunctival fornix, it takes about 20 minutes to perform. We prefer to use AmnioGraft (BioTissue) cryopreserved amniotic membrane tissue to restore the tear reservoir to its normal state and expedite the patient’s recovery. (Editor’s note: Dehydrated amniotic tissue such as Ambio2 Amniotic Membrane [Katena] can also be used in this type of ocular surface surgery.)
The cryopreserved amniotic membrane promotes quick healing with minimal postoperative discomfort; it helps reduce inflammation, promote regenerative healing, and suppress pain, and it achieves excellent cosmetic results (Figure 2). In our experience, about two-thirds of patients have enough clinical improvement that they request to have their fellow eye done after the first eye heals.
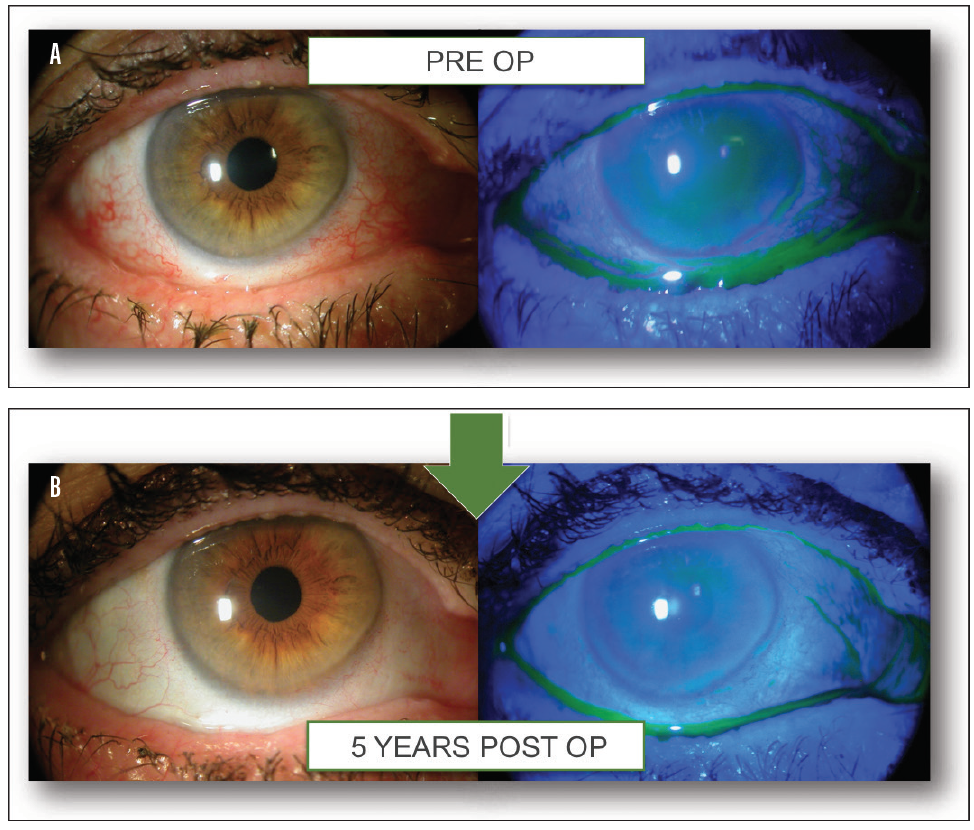
Figure 2. Before (A) and after (B) reservoir restoration, in which cryopreserved amniotic membrane is used to deepen the tear lake and restore the patient’s ocular anatomy to its normal state.
TEAM UP TO SUCCEED
When optometrists and ocular surgeons join forces to comanage patients with MDE, there are potential benefits for the patient, the provider, and the practice. Comanaging MDE patients offers the potential for practice building for several reasons. First, MDE is an extremely common condition among older patients. Second, patients are eager to find a solution to a problem that sometimes causes great discomfort. Third, the surgery is safe and fast. And finally, patients are generally sufficiently satisfied that they request surgery on their second eye.
Drs. Devries and Manning supervise the teaching center at Eye Care Associates of Nevada for the tear reservoir restoration procedure.
1. Mimura T, Yamagami S, Usui T, et al. Changes of conjunctivochalasis with age in a hospital-based study. Am J Ophthalmol. 2009;147(1):171-177.e1.
2. Qiu W, Zhang M, Xu T, et al. Evaluation of the effects of conjunctivochalasis excision on tear stability and contrast sensitivity. Sci Rep. 2016;6:37570.
3. Balci O. Clinical characteristics of patients with conjunctivochalasis. Clin Ophthalmol. 2014;8:1655-1660.



