

We work at a large OD-MD practice that specializes in both refractive and cataract surgery, so our schedules are full of patients at every stage of their surgical journeys. We have found that comanagement between our surgeons and their referring optometric colleagues, both internally and externally, is often best for our patients and for the referring practitioners.
In this article we aim to give readers the tools and knowledge needed to perform successful and comprehensive postoperative management of their LASIK referral patients.
AT A GLANCE
- At the postoperative day 1 visit, starting with binocular visual acuity can be helpful, as patients will see better this way and feel more of a sense of excitement about their vision.
- At the week 1 visit, 20/20 or better monocular VA is expected; patients with complaints of fluctuating vision should be reassured that this is common.
- At the month 1 visit, the patient’s vision should be at its best and fluctuation of vision minimal.
BEGINNING THE JOURNEY
To begin the post-LASIK comanagement journey, the referring OD must secure the patient’s approval for such management. We believe that it’s best for the doctor, when initially discussing LASIK surgery with an interested patient, to inform the patient that the necessary postoperative care can be provided in the OD’s office.
By also offering to coordinate the appointment with your preferred surgeon or surgical facility, you can help the process flow more smoothly for the patient. In addition, you’ll need to ensure that the patient will be released back to your care by the surgeon. This can be accomplished quite easily by having the surgeon sign a transfer-of-care agreement, which basically states that the surgery went as expected and that the surgeon is comfortable with all future care being managed by you.
FOLLOWING UP
How are the follow-up visits scheduled? What are the expectations for each visit? In the past at Williamson Eye Clinic, we have done postoperative visits at 1 day, 7 to 10 days, and at 4 to 6 weeks. Each surgeon typically has his or her own way of doing things, but they all generally follow this timeline. However, as the COVID-19 crisis has established new normals in all areas of health care, we have been exploring replacing the 1-day postoperative visit with a telemedicine call. Following is a description of what is involved in each of our major postoperative examinations.
1 Day Postop
We like to begin by congratulating the patient and reassuring him or her that everything is going well. As is the case in all of health care, patients love to hear that the surgery went well and that the healing process is moving along as expected. Next, we quiz patients in regard to any signs and symptoms they’re experiencing and then inquire about their use of the prescribed medications. Blurriness, burning, and tearing are common complaints on the first day after the procedure, and patients should be reassured that these are completely normal and should improve rapidly with time and the appropriate medications. (We discuss our typical drop regimen below.)
After taking a careful history, it’s time to check visual acuity. Starting with binocular vision can be helpful, as one eye may be much better than the other on day 1. Patients will see better this way and feel more of a sense of excitement about their vision. After that, a check of monocular vision is performed. We expect at least 20/40 vision at this visit, as the corneal swelling and healing process often limits acuity. If vision is superior to that, we make a point to inform patients that they are already seeing better than we expected at this visit. If vision seems unexpectedly off, a careful slit-lamp examination to look for complications is warranted.
We carefully examine for complications at this visit. If vision is unexpectedly poor (we use 20/60 as a reference point), this is typically a result of corneal dryness or, less frequently, a LASIK flap issue such as wrinkling or displacement (Figure 1). Corneal dryness typically manifests as a small amount of superficial punctate keratitis or a reduced tear meniscus.
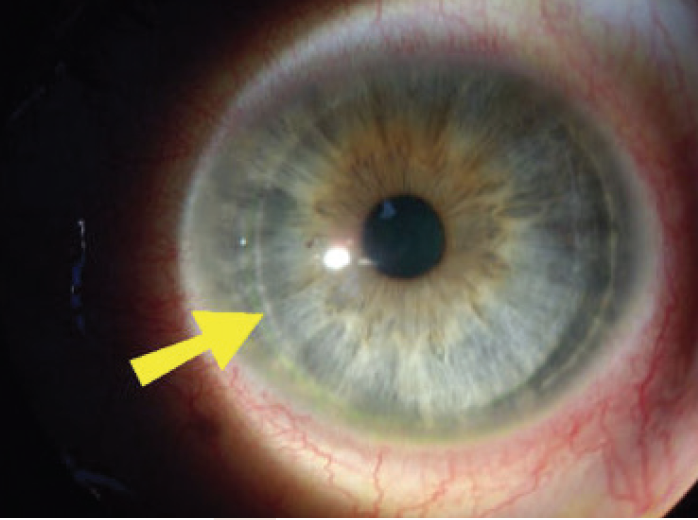
Figure 1. This patient may have only slightly to moderately decreased vision on day 1, but in this nasally hinged flap you can clearly note the large gap between the edge of the flap and the stromal bed. There is slight overriding of the flap over the inferior margin of the flap bed, which may continue to worsen if the flap is not lifted and repositioned immediately.
When we examine a LASIK flap, we look carefully at its position and relative smoothness. There should be no wrinkling or striae of the flap (Figure 2), and the edges of the flap should be well sealed and symmetrical along the periphery of the flap bed. There should be minimal or no anterior chamber reaction, and the interface between the flap and bed should be clear and free of debris.
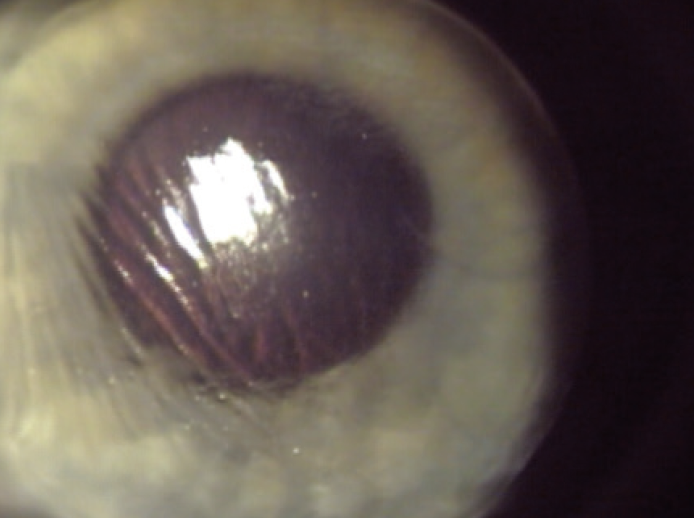
Figure 2. Note the significant striae in this flap, suggesting that it is not flush with the stromal bed, which will result in decreased and distorted vision. This is another indication for immediate flap repositioning. If the flap is left alone and heals improperly, chronic issues with visual acuity can develop, and there can be more complications involved with trying to fix the problem later on.
Postoperative dryness is the biggest complication of LASIK. We routinely treat it with use of a high-quality, preservative-free artificial tear; our clinic prefers FreshKote PF (Eyevance Pharmaceuticals). Patients who are predisposed to dry eye should already be on a moisturizing regimen, and some may already have had punctual plugs inserted or may be using a prescription drop such as lifitegrast ophthalmic solution 5% (Xiidra, Novartis) or a formulation of cyclosporine (either Restasis, Allergan; or Cequa, Sun Ophthalmics) to increase tear production.
A flap issue such as wrinkling or displacement is serious, and an immediate referral back to the surgeon for repositioning should be done that day. Uncommonly, an epithelial defect can present at a LASIK follow-up visit, and these can be treated simply by observation or with a bandage contact lens if the patient is experiencing significant discomfort.
Finally, we review the patient’s drop regimen. In our practice, patients are prescribed a broad-spectrum fluoroquinolone antibiotic, typically besifloxacin ophthalmic suspension 0.6% (Besivance, Bausch + Lomb) or ciprofloxacin, with one drop in each eye four times per day for 1 week after the procedure. The patient is also prescribed a corticosteroid eyedrop to help reduce postoperative inflammation. Prednisolone acetate 1.9% or difluprednate ophthalmic emulsion 0.05% (Durezol, Novartis) is typically used every 2 hours for the first 2 days, with a taper to four times daily for the next 5 days. A high-quality preservative-free artificial tear should be used every 1 to 2 waking hours for the first week, with the frequency tapered over the next several weeks.
We remind patients to avoid rubbing their eyes for the next few days and to avoid smoky or dusty environments. Two common questions we receive at the 1-day postop visit relate to swimming and makeup use. We recommend that patients wait at least 1 week before entering a pool or hot tub and that they avoid wearing eye makeup for approximately 1 week. If the patient notes discomfort or pain, we advise taking extra-strength (500 mg) acetaminophen every 4 to 6 hours as needed.
1 Week Postop
At this visit, 20/20 or better monocular VA is expected. Often patients have complaints of fluctuating vision during the first week due to dry eye, and they should again be reassured that this is common, as are the halos they see around streetlights and headlights. If worse than 20/30 VA is noted, a refraction is performed, and the patient is assured that the healing process is not finished.
It is also expected that by this visit the cornea will be clear and healthy. The flap will be well secured to the underlying stromal bed. So long as the cornea is clear and the flap interface looks appropriate, all prescription drops are discontinued. Any flap issues are treated as described for the 1-day postop visit.
If patients are happy with their ocular comfort and vision, they are simply reminded to continue their artificial tears two to four times each day and scheduled for a 1-month follow-up. If slit-lamp examination reveals any active inflammation, the patient is kept on the steroid for another 1 to 2 weeks depending on severity.
Aside from flap displacement, the most vision-threatening complication after LASIK surgery is diffuse lamellar keratitis (DLK), also known as Sands of Sahara syndrome. This is a noninfectious, sterile inflammatory process that results in significant visual disturbance and discomfort. The most common time for presentation of this condition is within the first 2 to 5 days after surgery, although delayed onset may occur. DLK will not be apparent in the first 48 hours, but a patient experiencing it will often be in our office with complaints before the routinely scheduled 1-week appointment. This pathology is based on a sterile inflammatory reaction with neutrophil infiltration of the flap-bed interface.
At the slit lamp, one will see whitish deposits in the periphery with little to no visual disturbance in minor cases of DLK, and diffuse deposits (sometimes with clumping of cells) with significant visual disturbance in severe cases. Severe DLK may induce stromal necrosis, and this is a vision-threatening emergency that should be treated with lifting and irrigation of the flap and bed, along with intensive use of a topical steroid. Minor cases are treated simply with frequent topical steroids and close reexamination until they resolve.
1 Month Postop
At the 4 to 6-week visit, the patient’s vision should be at its best and fluctuation of vision minimal. If visual acuity is worse than expected, the cornea should once again be checked for dryness or irregularities. A refraction is performed to assess residual error, which can later be corrected with an additional LASIK procedure if necessary.
Uncommonly, a patient may need temporary punctal plugs or the addition of lifitegrast or cyclosporine to encourage tear production. You will find that most patients have tapered their artificial tears to a level they are comfortable with. Because they are now experiencing excellent vision with no residual symptoms, this may often be the last follow-up appointment needed after LASIK.
If a patient requires plugs or additional medication, another follow-up is performed 4 to 6 weeks later. This will be just shy of, or at, the 3-month postoperative mark. Issues with dryness should be resolved and, if needed, a reliable refraction can now be performed. If vision is not up to the patient’s expectation and residual refractive error exists, a LASIK touchup can now be offered to fine-tune acuity.
Some patients, especially older patients or those with preexisting dry eye, should be reminded to continue the use of artificial tears at the level most comfortable for them. They must be made aware that long-term dryness is a major risk and that it may persist because we have structurally altered their corneas.
Once these examinations are complete, the patient may be scheduled for routine yearly exams to assess overall eye health, or sooner as needed to manage dry eye or other conditions.
COMANAGE WITH CONFIDENCE
We hope this article has provided you with the confidence to either begin the comanagement of LASIK surgery or to continue with increased confidence. By keeping patients in your practice and allowing them to witness your clinical acumen, it will undoubtedly aid in helping you to build the medical component of your practice.



