Collaborative care is all about communication. Communication between ophthalmologists and optometrists, communication between patients and doctors, and communication between office staffs are all critical to successful collaboration. However, it’s all too easy for a misstep to occur in the various routes of communication among these groups. The OD might say something inaccurate to the patient about surgical options, or the patient could misunderstand a comment the surgeon makes about a particular lens choice for surgery. It doesn’t take much to create a problem in what can already be a complex chain of interactions.
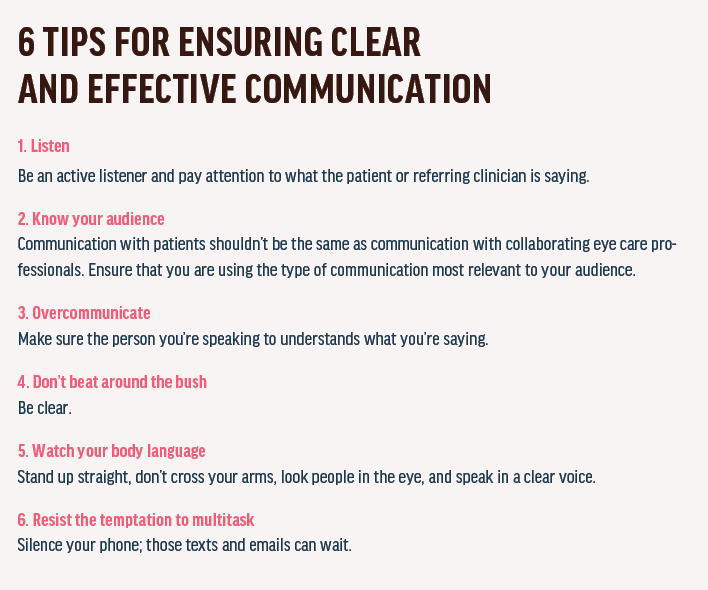
Following are some examples of scenarios where miscommunication might easily occur in today’s world of collaborative care. Read 6 Tips for Ensuring Clear and Effective Communication for some helpful pointers.
PRESBYOPIC IOLS: WHO CAN BENEFIT?
In a discussion of cataract surgery options, the optometrist says to a patient, “Mrs. Smith, there are some lenses used in cataract surgery that can give you both distance and near vision, but they don’t work well and they cost too much.” Meanwhile, across town, the surgeon thinks, “Some of my happiest patients have presbyopia-correcting lenses. Does he not want to bother, or is he worried about losing the glasses sale?”
In the dark ages (about 5 years ago), many optometrists would shy away from multifocal IOLs because they were tired of receiving complaints of glare, halo, and poor intermediate vision for computer work in patients who returned to their practice after cataract surgery. The headache of dealing with their patients’ visual side effects soured their perception of advanced IOLs.
The advent of low-add multifocals and extended depth of focus (EDOF) lenses gave us a fantastic way to meet the visual needs of our technology-savvy cataract patients. With EDOF lenses, patients experience less glare and better intermediate vision for activities on the computer.
As for that glasses sale, patients still often need a prescription for small print at near, and they can take advantage of the glasses benefit on their insurance policy for that.
Sometimes, however, there may be incorrect beliefs or myths floating around among referring optometrists. Some may overstate the benefits of a particular presbyopia-correcting lens, for example. We tell patients that our goal is to minimize dependence on glasses, not eliminate them entirely. There are many variables that can affect refractive results, we say. If patients go into surgery with the right expectations, the likelihood is high that they will be pleased with the results.
OCULAR SURFACE DISEASE: WHO DOES WHAT?
An optometrist sees a new patient with visually significant cataracts and moderate dry eye syndrome and refers the patient to the surgeon for treatment. The surgeon, thinking that the OD can manage the dry eye postoperatively, proceeds with surgery without much discussion of the condition with the patient. After surgery, the unhappy patient tells the referring OD that her vision is no better than before.
This is a hot topic right now in refractive cataract surgery. We are now all aware that tear film abnormalities can greatly affect cataract surgical outcomes. In the PHACO study, Trattler et al found that 77% of patients presenting for cataract surgery had grade 2 or greater dry eye disease.1 And we know, from a study by Epitropoulos et al, that dry eye disease is associated with a higher percentage of IOL power calculation errors greater than 1.00 D.2 This is why we see refractive surprises, as biometry readings can vary greatly in patients with dry eyes. Many patients are mildly symptomatic, however, and it can be difficult to convince them to delay surgery when they desire immediate removal of their cataracts.
Treating dry eye even slightly before surgery is crucial to increase the likelihood of a satisfied patient postoperatively. But the job is not yet done. We now have advanced dry eye diagnostic testing methods, including measurement of tear osmolarity and certain inflammatory markers, allowing us to identify meibomian gland function and atrophy both preoperatively and postoperatively. As a result, we have become aware that, even in an eye treated preoperatively for dry eye, cataract surgery and its associated topical drop therapy tips the scale back toward dry eye postoperatively. On an already fragile ocular surface, this may be the straw that breaks the camel’s back.
When patients become increasingly symptomatic after surgery, it is likely that their meibomian gland dysfunction and ocular surface disease were preexisting preoperatively. Therefore, we have found that it is helpful to educate patients and initiate therapy targeted to the patient’s specific needs prior to cataract surgery.
LOOK A LITTLE DEEPER
About a year ago, a patient presented to our clinic for a second opinion, begging us to remove her toric IOL. It had been inserted 2 years prior at another practice, and the patient was in misery. She believed that her toric lens was creating fluctuating, smeary vision that she could not get to stay clear. She had seen five different surgeons in that other practice but had been offered only topical lubrication as a treatment option.
We performed our standard dry eye workup and informed the patient that her meibomian glands were blocked and that this was creating much of the symptoms she was experiencing. We performed vectored thermal pulsation (LipiFlow, Johnson & Johnson Vision) and encouraged her to return 2 months later. At that follow-up visit she was in tears, grateful that her vision had finally cleared and stayed clear. We have had multiple patient encounters like this, highlighting the importance of identifying and treating ocular surface disease early in the surgical pathway.
TEAMWORK MAKES THE DREAM WORK
We are fortunate to live at a time when collaboration between ophthalmologists and optometrists continues to grow. Communication is crucial, and, with the rapidly changing landscape of surgical ophthalmologic management, it is important for referring optometrists to correctly inform patients so that misinformation and miscommunication are minimized.
Ophthalmologists love it when referring optometrists shadow us at our surgical centers. This activity provides them with continuing education credits and allows them to ask questions one-on-one regarding surgical options. It also fosters trust and open communication toward our mutual goal of improving and restoring visual function in our shared patients.







