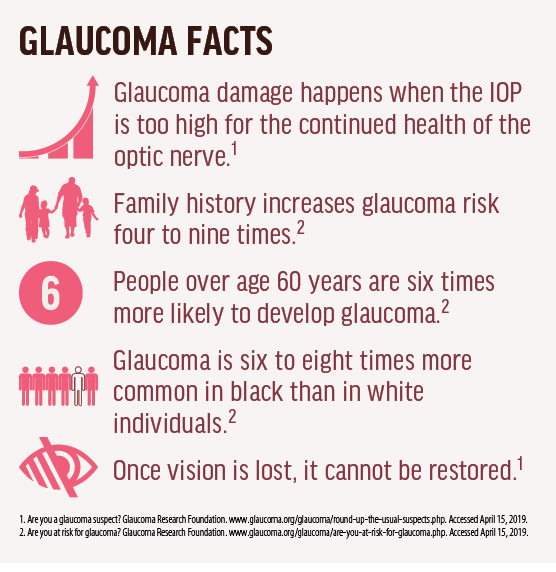
Early detection of glaucoma is essential to preserving patients’ functional vision. Piecing together the most appropriate assessment after weighing all the data collected is an art that is in many ways unique to glaucoma. The decision to categorize the patient as a glaucoma suspect as opposed to a patient with definitive glaucoma can be challenging, especially when the patient is new to the clinic. Clinical experience is an important asset. I often return to the description of glaucoma as a neurodegenerative disease that presents itself at various stages of a continuum.1
If a patient is a glaucoma suspect, the next most important factor to clearly identify is the risk of his or her progression to glaucoma. Is this patient a high-risk glaucoma suspect or at low risk of developing glaucoma? If the patient has definitive glaucoma, what is the most accurate placement of this patient on the glaucoma continuum?
Putting the patient in the right bucket—glaucoma patient versus glaucoma suspect—and understanding the overall risk to functional vision begins with basic yet important investigations. This article reviews some of the factors that I consider with every patient who comes into my clinic for a glaucoma evaluation.
HIGHEST MEASURED IOP (T-MAX)
A patient with a moderately high IOP can often be one who needs only careful surveillance. This is often the case in the early postoperative period after routine or complex surgery. Understanding the setting in which that T-max reading was collected is crucial. If we measure and document a high T-max without significant precipitating factors, it becomes an important reference point for effectiveness of treatment if the patient goes on to develop glaucoma.
In the absence of additional risk factors, T-max is a strong indicator that a patient is at risk of developing preperimetric glaucoma. IOP is the only modifiable risk factor for glaucoma. Flattening the IOP diurnal curve and minimizing spikes is crucial for preservation of the optic nerve.
I look forward to publication of more data on the accuracy of at-home IOP-monitoring devices. If we could have patients coming to us with a 3-month report of daily IOP measurements rather than one data point twice a year, that would significantly help us fine-tune our treatments and match patients with IOP-lowering drops that might have a greater impact during the times of day that the patient is most at risk.
FAMILY HISTORY
Does the patient have a family history of glaucoma? If so, do his or her parents have glaucoma, and how many siblings have glaucoma? For example, if a patient’s father and two of five siblings have glaucoma, I would monitor the patient more closely in the absence of pertinent clinical findings, compared with a patient who might have the same risk factors but no family history. As I review the charts of my patients who fall into this category of glaucoma suspects (with notable family history, yet no definitive signs confirming conversion to glaucoma), there is a common factor that ends up playing a key role in the decision to treat: accurate IOP measurement. I often find a significant discrepancy when I retest it myself. There are many reasons why it might be inaccurately measured, including deep, inset globe; strong orbicularis; or anxiety, but I find the most common reason to be staff turnover. Technicians who are not yet fully trained can misread this critical data point. As providers, we have to be vigilant here. Following these patients every 6 months is reasonable, and I make sure to measure IOP a second time myself. IOP is still our single modifiable risk factor in glaucoma, so we had better start with an accurate data point.
Similarly, it is helpful to find out the severity of disease in family members. For example, has the father had multiple glaucoma surgeries? Is there blindness due to glaucoma in the family? I often find that patients I have been treating for years also have family members who have a history of trabeculectomy or tube shunt and are seeing our glaucoma surgeons. This is another factor in my mind that is a reminder to stay ahead of IOP fluctuations in these patients because they’ve had family members with glaucoma that was aggressive enough to cause blindness and require surgery.
SYSTEMIC HEALTH
Evaluate the patient’s blood pressure and body mass index, and ask whether the patient has obstructive sleep apnea (OSA). Symptoms of OSA can be underreported by patients, contributing to its underdiagnosis and undertreatment.2 Multiple clinical studies have identified a higher prevalence of glaucoma in patients with OSA.2
If the patient does have this condition, it’s important to try to understand whether the patient is compliant with his or her OSA treatment. In my experience, patients who report inconsistent compliance or noncompliance with OSA treatment are likely to behave the same way regarding a glaucoma therapeutic regimen.
PREVIOUS REFRACTIVE SURGERY
In patients with previous refractive surgery, double-check to make sure your tech team is not just pulling forward old pachymetry readings. If this is overlooked, it can have significant implications in risk factor calculations. An accurate pachymetry reading is essential in the list of considerations that we calculate when considering the initiation of treatment. Treatment for a particular patient may have been more appropriate earlier when his or her central corneal thickness was thinner.
TARGET IOP
When you initiate treatment for a patient with glaucoma or ocular hypertension, it is important to set an appropriate target IOP. Use the target as a reference point for nerve fiber layer and visual field stability.
When IOP-lowering treatment is initiated, define a target IOP, but remember that it isn’t set in stone. This is important for long-term preservation of functional vision. For example, if a goal of 20% reduction in IOP is achieved in treatment of an early glaucoma patient, but progressive visual field changes are detected on follow-up, the clinician should react to these changes and lower the IOP further.
Sometimes the clinician may inherit a glaucoma patient from another practitioner or see a patient for an interim IOP check and note that the target pressure has not been achieved. In these instances, we need to stick to the previously defined target, even if there hasn’t been any vision loss since the last visit. If we’ve carefully considered the severity level of the glaucoma patient, the T-max, the patient’s age, and his or her glaucoma risk factors, use of a target pressure should be considered the standard of care.
THREE QUESTIONS
I find that the considerations discussed above are crucial in helping me understand the following three mandatory questions for every glaucoma patient:
Question No. 1. What is this patient’s risk of developing glaucoma?
Question No. 2. What is this patient’s risk of functional impairment due to glaucoma?
Question No. 3. What are the best treatment options for this patient?
With an expanding set of treatment options available to us, IOP-lowering drops may not always be the best first choice for many older patients. Optometrists are well positioned to discuss microinvasive glaucoma surgery options with patients.
In addition to the considerations above, adherence to topical medication regimens is still a key factor for vision preservation in glaucoma.4 Unfortunately, we’ve all had patients lose vision to glaucoma. As I look back at my charts for these patients, deviation outside of the target determined to be a safe IOP is common. But sadly, I also often see notes in these patients’ charts referring to suboptimal compliance. This is especially frustrating when patients lose vision.
When I prescribe drops, I try to get ahead of potential tolerability issues by stressing to the patient the importance of communicating any symptoms back to my office. This is particularly vital at the beginning. Despite our best efforts, sometimes patients will come in for a 3-month IOP check with uncontrolled IOP because they stopped their medications due to intolerance.
One of the best indicators that a patient may be at risk of drop intolerance is the presence of ocular surface disease (OSD). This is best identified in a thorough initial assessment. I treat OSD aggressively in all of my glaucoma patients for this reason. It helps to have patients come in for an initial, separate visit focusing on their OSD so that we can spend the appropriate time identifying and discussing the OSD treatment strategy.
This can also be a balancing act, as OSD therapy itself can add up and can become onerous and costly. However, this emphasis on OSD can be worth the effort. In my experience, it is often the case that patients can be at risk of vision loss because of failure to use IOP-lowering drops due to OSD-related issues.
IT PAYS TO KNOW
Glaucoma is a complex disease that requires vigilance and dutiful preparation in order to arrive at the best treatment plan. Patients with mild glaucoma require significant attention to keep them in that category. The first step is accurately determining whether your patient is a suspect or a verified glaucoma patient. If you master this critical skill, you’ll have a stronger chance of keeping your patients at the mild severity level and helping them live full, productive lives, even if they develop glaucoma eventually.
- Weinreb RN, Friedman DS, Fechtner RD, et al. Risk assessment in the management of patients with ocular hypertension. Am J Ophthalmol. 2004;138(3):458-467.
- Chaitanya A, Pai VH, Mohapatra AK, Ve RS. Glaucoma and its association with obstructive sleep apnea: A narrative review. Oman J Ophthalmol. 2016;9(3):125-134.
- Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701-713.
- Okeke CO, Quigley HA, Jampel HD, Ying GS, Plyler RJ, Jiang Y, Friedman DS. Adherence with topical glaucoma medication monitored electronically: the Travatan Dosing Aid study. Ophthalmology. 2009;116(2):191-199.