MEIBOGRAPHY IN A YOUNG PATIENT
By Alice Epitropoulos, MD; and Marjan Farid, MD
Don’t make the mistake of assuming that meibomian gland dysfunction (MGD) affects only the elderly. Preoperative cataract and refractive surgery patients and dry eye disease patients should undergo dynamic meibomian gland imaging to evaluate their gland structure. In our practice, we use the LipiView II Ocular Surface Interferometer (Johnson & Johnson Vision) for dynamic meibomian imaging; other platforms include the Meibo-scan function on the Keratograph 5M (Oculus) and the Meibox imaging platform (Box Medical Solutions).
Gland shortening and tortuosity are early signs of MGD; gland dropout occurs at more advanced stages. Figure 1 shows significantly affected gland structures in the right eye of a young woman. Alterations in meibomian gland morphology and function due to contact lens wear can linger even years after discontinuation.1 Reduced blinking with use of digital devices, which can lead to ocular discomfort and vision problems often referred to as computer vision syndrome, likely contributes to MGD in young, screen-active patients.
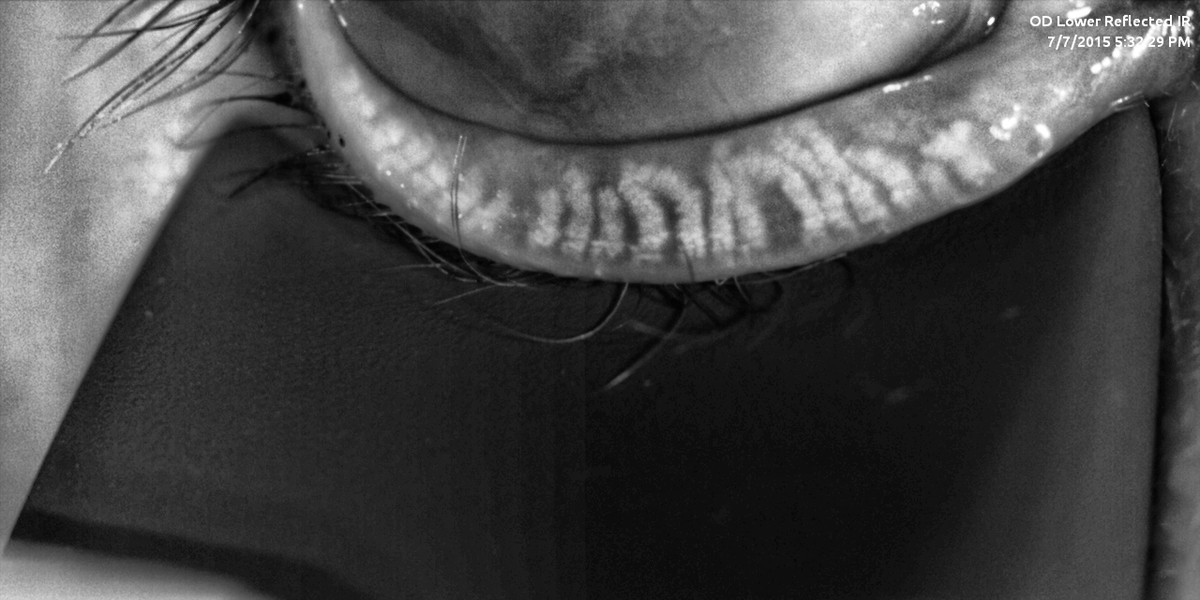
Figure 1. Meibomian gland imaging shows evidence of pathologic gland structures.
Showing patients their own meibography images and comparing them with meibography images from a healthy eye can be a very effective way to improve the patient’s understanding of the condition and secure their engagement with therapeutic recommendations. Treatment of MGD in young patients may allow those patients to resume contact lens use, become better candidates for laser vision correction, and improve their quality of life.
And, perhaps most important for some young patients, it may allow them to more comfortably work on their digital devices.
- Alghamdi WM, Markoulli M, Holden BA, Papas EB. Impact of duration of contact lens wear on the structure and function of the meibomian glands. Ophthalmic Physiol Opt. 2016;36(2):120-131.
EDUCATION AFTER CONCUSSION
By Cathy Stern, OD
Patients with conditions that affect binocular vision, reading vision, or sports-related vision may find it difficult to conceptualize the relationship between the brain and the eyes, or between therapy and progress. Patients who report vision problems may have an oculomotor dysfunction or an undiagnosed concussion. For both types of patients, the RightEye eye-tracking system (RightEye) can be used to educate patients about their conditions by providing quantitative data in a take-home report (Figure 2).
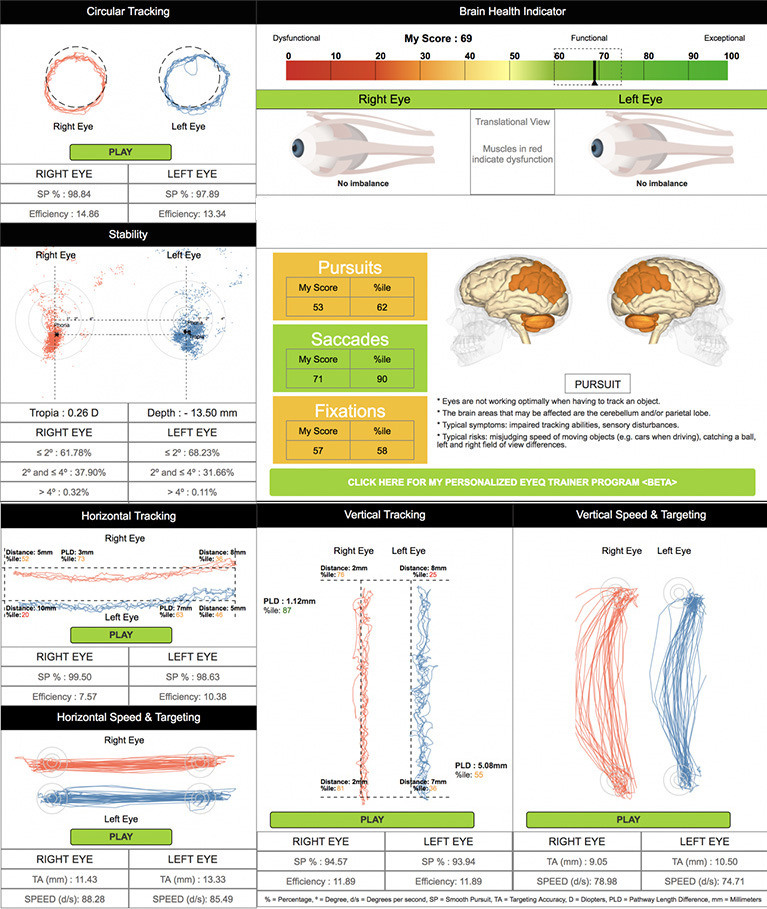
Figure 2. An example of the EyeQ patient report.
Patients who use the platform participate in a series of short, game-like tests that measure core functional vision skills such as reaction time, stability, and smoothness of eye movements. The device then summarizes the patient’s oculomotor performance and displays the quantitative data in a personalized take-home EyeQ report. EyeQ includes easy-to-read graphs of test results and short descriptions that help patients understand their data.
Clinicians may use the EyeQ report as an educational tool during posttest consultations. The report’s visual elements and graphs can help improve the patient’s understanding of his or her condition. Because it goes home with the patient, the report may improve the patient’s retention of test results, help him or her explain their condition to others, and lead to better therapeutic compliance.
RightEye is used for treating, retesting, and monitoring a patient including those with concussion, to objectively measure the effects of their therapy. The EyeQ graphical reports are both a teaching tool and a measuring stick not available from other technology solutions.








