Whenever a new category is introduced, uncertainties and growing pains are to be expected. They are standard with the development of any novel technology or technique, and we are certainly experiencing this effect with the growth of microinvasive glaucoma surgery (MIGS).
To differentiate from traditional glaucoma filtering surgery, MIGS was defined as a group of surgical procedures that share five preferable qualities: (1) an ab interno approach, (2) minimal disruption of normal anatomy and physiology, (3) an extremely favorable safety profile, (4) at least modest efficacy, and (5) rapid patient recovery.1
Later, the FDA described MIGS as “a type of IOP-lowering device used to lower IOP using an outflow mechanism with either an ab interno or ab externo approach, associated with little or no scleral dissection and minimal or no conjunctival manipulation.”2
Over the past decade, several devices have been introduced to achieve the ultimate objectives of MIGS. Although different in design and function, these devices typically share some common ground. They are at least modest in efficacy. The goal of their implantation is not necessarily to lower IOP to below-normal range, but often to reduce medication burden while hitting modest IOP targets. These devices encompass a safety profile that yields quicker recovery, more reproducible results, and fewer postoperative visits. They are generally refractively neutral compared with traditional glaucoma surgery, and, in some cases, their efficacy may be worse; the tradeoff is increased patient safety.
THE PROBLEM WITH LABELS
Given the increasing number of treatment options and the variations among them, the MIGS category has become more challenging to clearly distinguish. But, in truth, categorization is rarely foolproof. Although a useful organizational tool, categorization can be misleading, especially if misinterpreted to imply homogeneity.
The classification of an object into a specific category does not dictate that all objects within that category should be exactly the same. Instead, it is a means to recognize and differentiate. And, generally, all of these procedures ought to be distinguished from traditional glaucoma surgeries. For the most part, they are less invasive, safer, and associated with faster patient recovery.
But just because a device is classified as MIGS does not mean it adheres to a universal standard. Certainly, not all MIGS devices carry the same risk profile, ease of use, or patient population. No one device is universally applicable to or effective in all cases, and no one device is the safest, least invasive, and most effective of them all. We must balance safety, efficacy, and invasiveness, and there will likely be a tradeoff for the foreseeable future, as no device excels in all realms.
Thus, we must collectively reject the notion that every surgeon should have his or her “go-to” MIGS option. In fact, as we enter an era when MIGS is not only customizable to the patient but to each eye, it is all the more important that we recognize a place for multiple treatment options within this shared space.
THE MATURATION OF MIGS
Developing a new category is analogous to raising a child. At birth, the excitement and novelty are strong. Then, as it enters “adolescence,” the struggle to find its identity ensues. If we had to wage a bet, we’d say that, currently, MIGS is working its way through these confusing “preteen to teenage years.” It is struggling to figure out exactly who it is and who it is meant to be. But, rest easy, in a couple of years, more data will be collected, and MIGS will “turn 18.” At that point, there will be data for each device, and the next phase will be comparative analysis within the devices themselves.
Once MIGS reaches maturity around “middle age,” that is when it will be truly customizable. We will have maximized the use of the devices, and we know what we’ll get with each. As MIGS continues to age from this point, we will have a clear understanding of how it is going to react in any given situation … but good luck trying to change it.
For now, we’ll keep celebrating each milestone and the fact that this category exists at all. It may be a bit of a confused teenager at the moment, but weren’t we all once (Figure)?
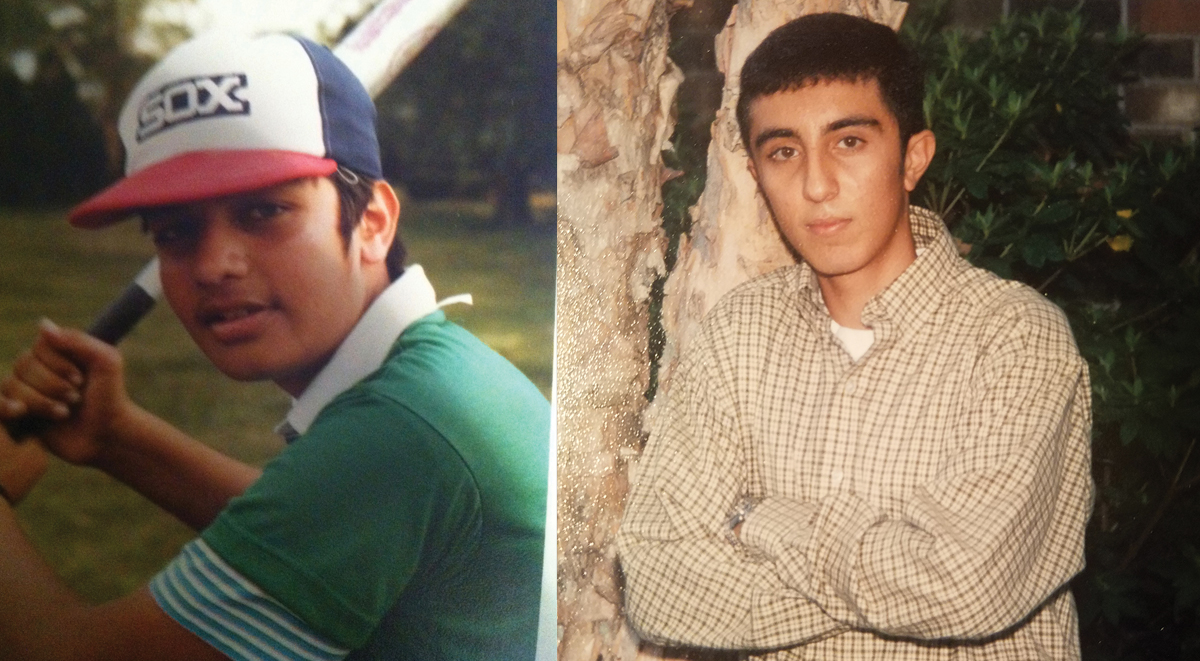
Figure. The authors as confused teenagers: Iqbal Ike K. Ahmed, MD, FRCSC (left), and Arsham Sheybani, MD (right).
- Saheb H, Ahmed IK. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23(2):96-104.
- Premarket studies of implantable minimally invasive glaucoma surgical (MIGS) devices: guidance for Food and Drug Administration staff. US Food and Drug Administration. December 15, 2015. bit.ly/2L95zwp. Accessed July 1, 2018.