The importance of the ocular surface to outcomes of refractive cataract surgery cannot be overstated. Now more than ever, surgeons’ ability to optimize patients’ vision after surgery depends on the state of the cornea’s health before the procedure. To meet high patient expectations and justify the high costs of premium IOLs, eye care providers must evaluate patients for and treat dry eye disease (DED) before surgery and ensure that they have a healthy ocular surface preoperatively. The incidence of DED increases with age, and it is well recognized that DED can disrupt preoperative calculations and tests and affect postoperative visual quality.
A patient referred to me illustrates the importance of the findings of the PHACO study, which assessed the effect of DED in refractive cataract surgery.1 The study found that the incidence of DED in patients scheduled to undergo cataract surgery was higher than anticipated (see sidebar, PHACO). Had an eye care provider identified DED in this patient and treated it preoperatively, she might have been happier with the surgical outcome.
A CASE OF UNHAPPINESS
A 67-year-old woman came to my office for a second opinion. She was extremely unhappy after her premium IOL surgery. She stated that she had paid a significant amount out of pocket for the implant, and it was, in her words, “a waste of money.” She claimed that her distance and near vision were both bad, and that she was disappointed with her quality of vision overall. She noted glare and halos immediately after surgery, and they never fully resolved.
Another ophthalmologist had told her she was a candidate for premium technology, as she had a visually significant cataract, minimal astigmatism, and a normal retina examination on optical coherence tomography (OCT). Her surgery with the »Tecnis Symfony extended depth of focus IOL (Johnson & Johnson Vision) was uneventful.
The patient wanted to know if she should have the IOL removed. My staff and I performed a full evaluation, including refraction, topography, OCT examination of the macula, and a DED workup. The patient had minimal cylinder, a normal OCT, a clear capsule, and a well-located IOL. She also showed signs of significant DED.
The patient had significant dropout on corneal topography, a cardinal indicator of DED (Figure). Her tear osmolarity was elevated at 327 mOsm/L in the right eye and 311 mOsm/L in the left eye. Lissamine green conjunctival staining was 2+, and corneal staining with fluorescein was 1+. The meibomian glands were moderately occluded, and tear breakup time was 4 seconds.
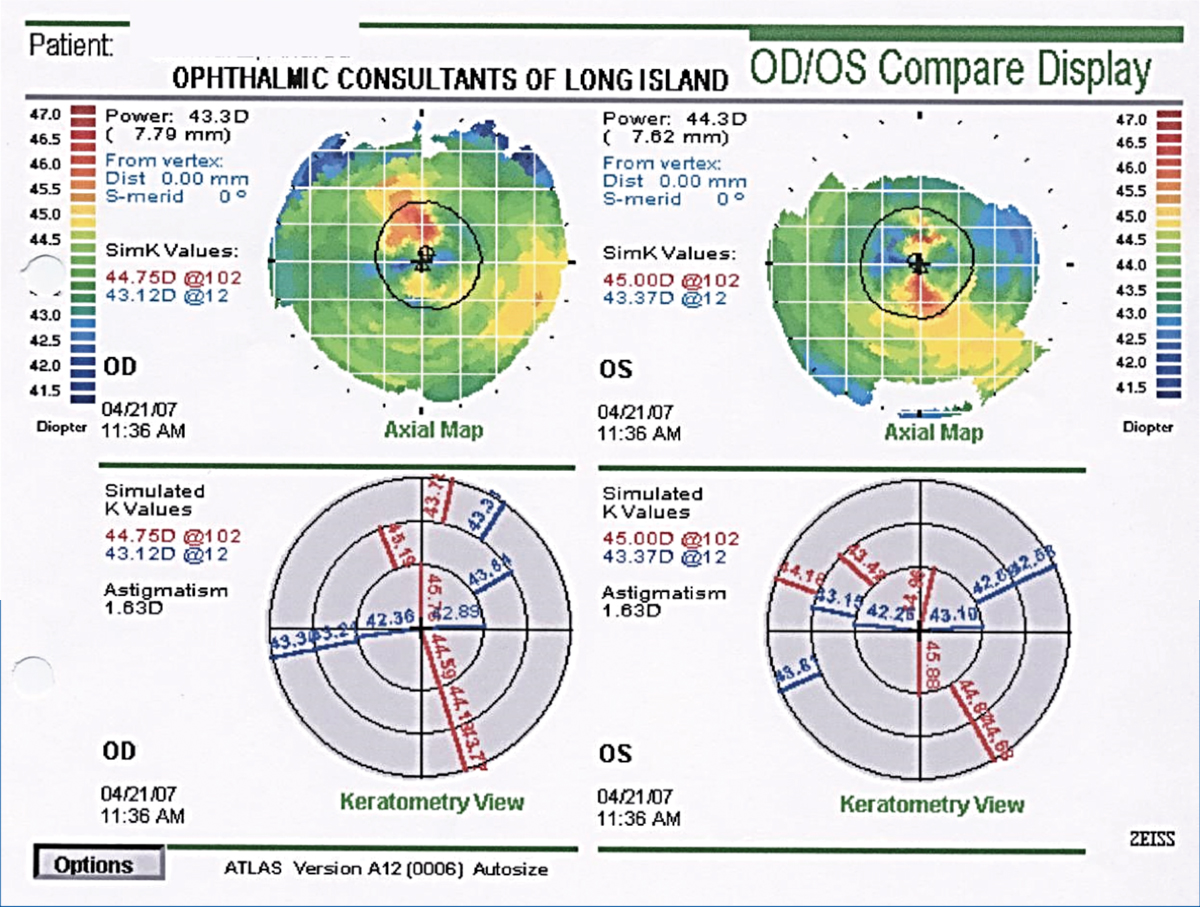
Figure. The patient's corneal topography revealed an irregular ocular surface suggestive of DED.
We managed this patient’s significant DED aggressively using warm compresses, »LipiFlow thermal pulsation treatment (Johnson & Johnson Vision), loteprednol 0.5% (»Lotemax; Bausch + Lomb) four times daily, lifitegrast 5.0% (»Xiidra; Shire), and artificial tears.
Within 2 weeks, the patient’s ocular surface resolved. Concurrently, her UCVA improved by 2 lines from 20/30+ to 20/20+, and her near vision improved by 3 lines. Corneal topography showed evidence of improvement as well.
CONCLUSION
In my experience, the Tecnis Symfony IOL usually presents few issues for patients. When I noted that this patient’s lens was indeed in good position, it was obvious that something else was responsible for her dissatisfaction. Now she is a happy presbyopic IOL patient.
One cannot perform premium cataract surgery using premium lenses without ensuring a premium ocular surface. Paying attention to ocular surface health is the most important thing surgeons can do to improve their outcomes.
- Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.