Pseudophakic cystoid macular edema (CME), also known as Irvine-Gass syndrome, results in painless vision loss and typically presents 4 to 6 weeks after cataract surgery, although risk factors for this complication can often be identified much earlier. Patients at heightened risk for CME include those with diabetes mellitus in the absence of retinopathy, those with diabetes with retinopathy (relative risk [RR] 1.80 and 6.23, respectively), patients with a history of epiretinal membrane (RR 5.60) or uveitis (RR 2.88), and those with retinal vein occlusion (RR 4.47).1
Educating patients who are at increased risk for CME before the procedure is important, as it will help to ease their consternation should the complication occur. Certain intraoperative complications, such as posterior capsular rupture and retained lens material, are also known to increase the incidence of CME.2 Should the patient experience any of the above, frequent dilation in the postoperative period may be indicated to aid in the detection of signs of CME.
Following are some pearls to keep in mind when you are comanaging cataract surgery patients.
RED FLAGS
Proposed etiologic factors for postoperative CME include inflammation, vitreomacular traction, and vascular instability. The primary etiology appears to be unregulated inflammatory mediators in the aqueous and vitreous as a result of surgical manipulation. These mediators (eg, leukotrienes and prostaglandins) disrupt the blood-aqueous and blood-retina barriers, leading to increased permeability.3 The timing of the typical onset of CME may be due to how long it takes for these inflammatory mediators to reach the back of the eye from the anterior segment.
Suspicion for CME is prompted by reduced VA or metamorphopsia that cannot be explained by other etiologies associated with cataract surgery, including residual refractive error, corneal edema, lens malposition, or posterior capsular opacification.
Visually significant CME is relatively uncommon, occurring in 0.1% to 3.5% of eyes following cataract surgery.4-6 Non–visually significant macular edema is much more common. It is seen in 3% to 41% of eyes evaluated with OCT and in 20% to 55% of eyes evaluated with fluorescein angiography.7
The patient’s VA and symptoms should determine the need for OCT imaging. Blurred vision in the absence of other findings requires careful dilated fundus examination and macular OCT (Figure 1). Routine imaging of all patients may identify some with asymptomatic CME and lead to unnecessary treatment and patient angst.
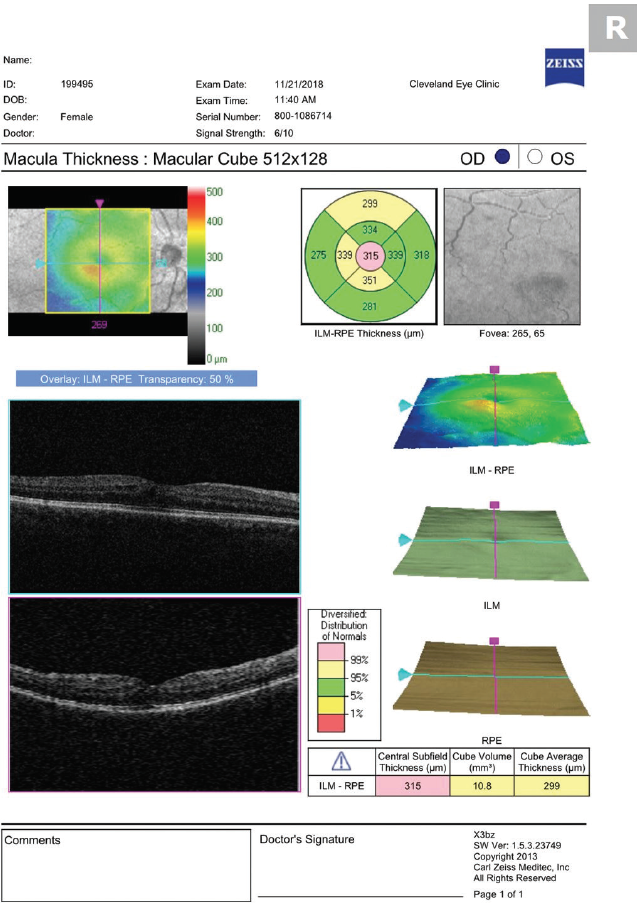
Figure 1. OCT performed 30 days after cataract surgery shows mild CME.
TREATING CME
There is no consensus that defines the optimum need for prevention or treatment of CME. Prophylactic treatment with a topical nonsteroidal antiinflammatory drug (NSAID) before cataract surgery was found to reduce the incidence of CME postoperatively; however, the visual effects of CME that did occur were insignificant in the long term (>3 months).8
Recently, dexamethasone intraocular suspension 9% (Dexycu, Eyepoint Pharmaceuticals) received FDA approval for injection behind the iris at the time of cataract surgery. This formulation was found to be safe and effective in treating inflammation occurring after cataract surgery and may be an alternative to postoperative steroid drop instillation.9
Prophylactic postoperative topical antiinflammatory medications reduce the incidence of CME. An analysis of 30 randomized clinical trials, including uncomplicated cataract surgery in nondiabetic patients, demonstrated that postoperative topical NSAIDs significantly reduced the odds of developing CME compared with postoperative topical corticosteroids.10 That analysis also found that a combination of corticosteroids and NSAIDs was superior to topical corticosteroids alone.
Should a patient develop CME despite prophylactic treatment, the condition can generally be managed with topical medications. Although the edema is often self-limiting over the course of several months, topical NSAID therapy is effective in reducing CME detected by OCT and may accelerate visual recovery after surgery compared with placebo.11 The combination of a corticosteroid and an NSAID also appear to be superior to either antiinflammatory medication alone. In one study, the average improvement in Snellen VA over 3 months was 1.6 lines in patients receiving an NSAID, 1.1 lines in patients receiving a steroid, and 3.8 lines in patients receiving a combination.12
In our practice, we prescribe prednisolone acetate 1% and ketorolac 0.5% to be used four times a day until resolution of CME, followed by a 3-week taper. We taper both at the recommendation of the retina group we work with (three times a day for 1 week, then twice a day for 1 week, followed by once a day for 1 week). Do not be alarmed if the severity of CME worsens just after beginning topical therapy. Similar to the delayed onset of the edema (surmised to be due to the time it takes for inflammatory mediators to reach the retina from the anterior segment), it also takes time for medications to reach the retina from the ocular surface (Figures 2 and 3).
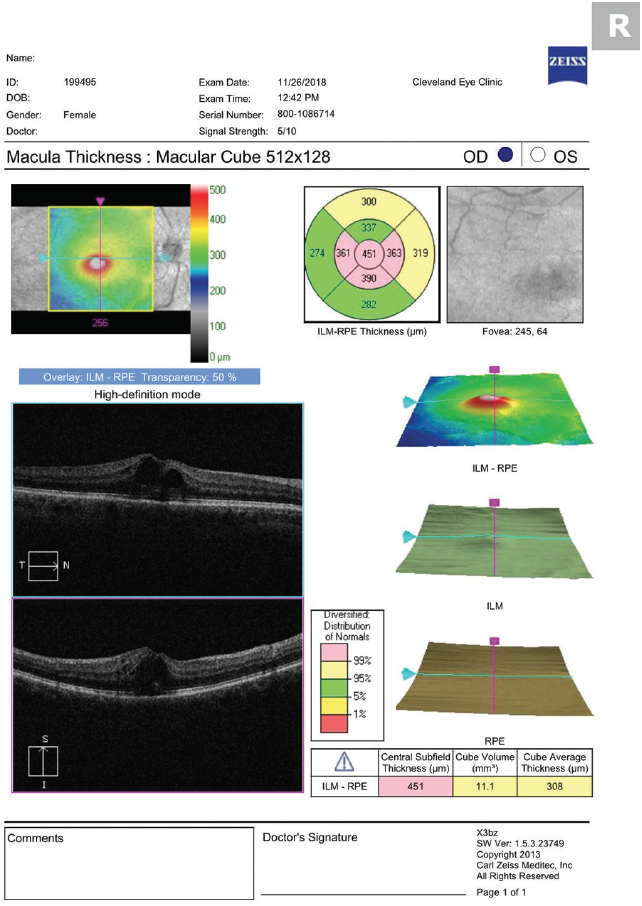
Figure 2. OCT performed 5 days after beginning treatment with prednisolone acetate and ketorolac four times a day shows worsening CME.
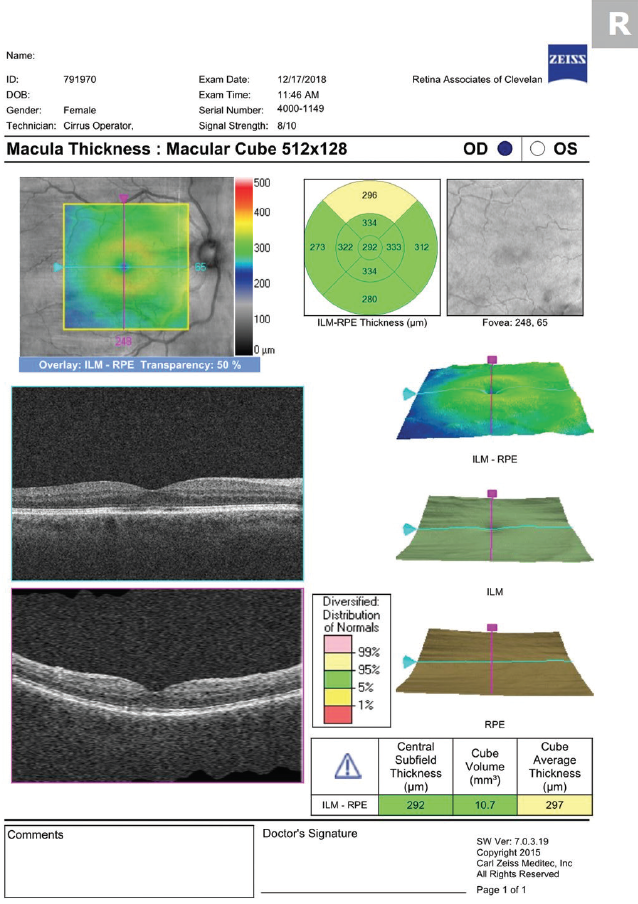
Figure 3. OCT performed 1 month after beginning treatment demonstrates resolution of CME.
Recalcitrant CME often requires further intervention for visual recovery. If structural (OCT findings) and functional (VA) improvements do not occur within 1 month of topical treatment, referral to a retina specialist is indicated. Periocular steroid injections (sub-Tenon and retrobulbar) have been shown to reduce edema and improve VA in CME refractory to topical treatment.13 Intraocular steroid injections and extended-release intravitreal implants have also improved outcomes in patients with chronic CME.14
Anti-VEGF injections have also been shown to be beneficial for the treatment of chronic CME. A multicenter retrospective study found that 72% of eyes with refractory CME treated with at least one intravitreal injection of bevacizumab (Avastin, Genentech) had improvement in VA and a reduction in mean central macular thickness at 12 months.15
In some instances, surgical methods must be employed to treat CME. For example, surgical removal of retained lens material may be needed to resolve recalcitrant CME. Pars plana vitrectomy has also resulted in improved visual outcomes for CME that has failed to respond to medical therapy.16
TAKE-HOME POINTS
In the comanagement of cataract surgery patients, it pays to be able to recognize common complications such as CME and to know how to proceed when they are detected.
To summarize, identify patients at risk (those with diabetes, epiretinal membrane, uveitis, or retinal vein occlusion) preoperatively. Also be aware of intraoperative complications that may increase the risk of CME (eg, posterior capsular rupture, retained lens fragments). Rule out other causes of postoperative blur, and perform a careful dilated exam and macular OCT to identify CME. Educate and reassure the patient that CME is a treatable condition. Treat topically with NSAIDs and steroids, and refer to a retina specialist for further intervention if CME is recalcitrant.
1. Henderson BA, Kim JY, Ament CS, Ferrufino-Ponce ZK, Grabowska A, Cremers SL. Clinical pseudophakic cystoid macular edema. Risk factors for development and duration after treatment. J Cataract Refract Surg. 2007;33(9):1550-1558.
2. Kim SJ, Belair ML, Bressler NM, et al. A method of reporting macular edema after cataract surgery using optical coherence tomography. Retina. 2008;28(6):870-876.
3. Benitah NR, Arroyo JG. Pseudophakic cystoid macular edema. Int Ophthalmol Clin. 2010;50(1):139-153.
4. Powe NR, Schein OD, Gieser SC, et al. Synthesis of the literature on visual acuity and complications following cataract extraction with intraocular lens implantation. Cataract Patient Outcome Research Team. Arch Ophthalmol. 1994;112(2):239-252.
5. Greenberg PB, Tseng VL, Wu WC, et al. Prevalence and predictors of ocular complications associated with cataract surgery in United States veterans. Ophthalmology. 2011;118(3):507-514.
6. Clark A, Morlet N, Ng JQ, et al. Whole population trends in complications of cataract surgery over 22 years in Western Australia. Ophthalmology. 2011;118(6):1055-1061.
7. Bélair ML, Kim SJ, Thorne JE, et al. Incidence of cystoid macular edema after cataract surgery in patients with and without uveitis using optical coherence tomography. Am J Ophthalmol. 2009;148(1):128-135.
8. Grzybowski A, Kim SJ. Corticosteroids substituted by nonsteroidal antiinflammatory drugs: is it justified by evidence-based medicine? J Cataract Refract Surg. 2016;42(3):510-511.
9. Donnenfeld E, Holland E. Dexamethasone intracameral drug-delivery suspension for inflammation associated with cataract surgery: a randomized, placebo-controlled, phase III trial. Ophthalmology. 2018;125(6):799-806.
10. Heier JS, Topping TM, Baumann W, et al. Ketorolac versus prednisolone versus combination therapy in the treatment of acute pseudophakic cystoid macular edema. Ophthalmology. 2000;107(11):2034-2039.
11. Kim SJ, Schoenberger SD, Thorne JE, Ehlers JP, Yeh S, Bakri SJ. Topical nonsteroidal antiinflammatory drugs and cataract surgery: a report by the American Academy of Ophthalmology. Ophthalmology. 2015;122(11):2159-2168.
12. Shelsta HN, Jampol LM. Pharmacologic therapy of pseudophakic cystoid macular edema: 2010 update. Retina. 2011;31(1):4-12.
13. Benhamou N, Massin P, Haouchine B, Audren F, Tadayoni R, Gaudric A. Intravitreal triamcinolone for refractory pseudophakic macular edema. Am J Ophthalmol. 2003;135(2):246-249.
14. Bellocq D, Korobelnik JF, Burillon C, et al. Effectiveness and safety of dexamethasone implants for post-surgical macular oedema including Irvine-Gass syndrome: the EPISODIC study. Br J Ophthalmol. 2015;99(7):979-983.
15. Arevalo JF, Maia M, Garcia-Amaris RA, et al; Pan-American Collaborative Retina Study Group. Intravitreal bevacizumab for refractory pseudophakic cystoid macular edema: The Pan-American Collaborative Retina Study Group results. Ophthalmology. 2009;116:1481-1487.
16. Cardone S, et al. The role of pars plana vitrectomy for pseudophakic cystoid macular edema. Invest Ophthalmol Vis Sci. 2003;44(7):3012.




