

Recent epidemiologic studies have identified a higher prevalence of keratoconus than previously reported, but even a conservative estimate of one in 2,000 suggests that there are nearly 4 million individuals with keratoconus worldwide. The development of corneal collagen crosslinking (CXL) has been a game-changer for these individuals’ quality of life.1,2 Before this procedure became available, eye care providers monitored patients, prescribed specialty contact lenses, and hoped that corneal transplantation would not become necessary.
AT A GLANCE
- The primary goal of CXL is to arrest the progression of corneal ectasia; once stability is achieved, there are several refractive tools available to improve vision.
- Patients with keratoconus that is detected early and stabilized with CXL can benefit from updated glasses prescriptions.
- Surgical corneal reshaping treatments aim to regularize corneal shape after CXL.
- Specialty lens fitting continues to be life-changing for patients with keratoconus after CXL or after CXL and surgical corneal reshaping treatment.
Current CXL technology has been shown to be highly efficacious in stabilizing corneal ectatic diseases and delaying or potentially eliminating the need for corneal grafts. Notwith-standing, it’s important to educate patients that CXL is primarily a means of halting disease progression and that mild improvement in visual acuity from corneal flattening may or may not occur. Given that these patients will still require visual rehabilitation to maximize their quality of life, this article will focus on optimizing the refractive care of patients with keratoconus who undergo CXL.
CURRENT STATE OF CXL
The only CXL technology so far to receive FDA approval is the KXL System (Glaukos). To learn about other technologies in the works, see CXL Options in the Pipeline. The KXL System was approved in 2016 for the treatment of patients with progressive keratoconus and post-LASIK ectasia using an epithelium-off (epi-off) technique.3 The FDA at the same time approved two topical ophthalmic solutions for use in CXL, riboflavin 5’-phosphate in 20% dextran ophthalmic solution 0.146% (Photrexa Viscous) and riboflavin 5’-phosphate ophthalmic solution (Photrexa), both available from Glaukos and both for use with the KXL System.
In the FDA-approved CXL protocol, the central 9 mm of epithelium is first removed under topical anesthesia. A riboflavin solution is then administered for 30 minutes, after which UV-A radiation is applied for another 30 minutes.3 Treatment creates singlet oxygen molecules that aid in forming covalent bonds, which act as crosslinks in the stromal collagen. At the conclusion of CXL treatment, a sterile bandage contact lens is placed on the eye to facilitate reepithelialization and enhance ocular comfort.
Again, the primary goal of CXL is to arrest the progression of corneal ectasia. The prospective multicenter clinical trial that supported FDA approval included more than 200 eyes with progressive keratoconus, half of which underwent CXL and half of which were monitored for some time prior to CXL (sham control). In the treatment arm, the maximum keratometry reading (Kmax) fluctuated during the first few months after CXL.4 A comparison of treated and untreated patients found a difference of 2.60 D in Kmax, with significant steepening in the sham control group and flattening in the CXL group. Often overlooked in discussions of this study is that slightly more than 50% of the patients who received CXL exhibited at least 1.00 D in Kmax flattening 12 months after treatment. A separate analysis found a similar result and reported that CXL successfully stopped corneal steepening.4
The safety profile of CXL in the FDA approval trial was good. The most common adverse event was corneal haze, which usually resolved by 3 to 6 months after treatment.4
THE REFRACTIVE TOOLBOX FOR CXL PATIENTS
Patients with keratoconus present excellent opportunities for collaboration between optometrists and ophthalmologists because these patients’ journeys typically begin and end in an optometrist’s office. Patients usually receive a diagnosis of keratoconus from an optometrist and return to that provider after CXL for optical rehabilitation and follow-up care (see Pearls for Collaborative Care).
Although other clinical options are slowly being adopted, there are four tools more commonly used in the current refractive toolbox for optical rehabilitation after CXL. Each one has pluses and minuses, as outlined below.
No. 1: Glasses and Soft Contact Lenses
Most patients with keratoconus will benefit from an updated glasses prescription after CXL.
Pros
When mild keratoconus is detected early, many patients can still enjoy functional vision with spectacle correction after CXL. Not only do glasses offer a convenience factor superior to that of most contact lenses, but glasses also allow contact lens patients to better comply with prescribed wear time.
Soft disposable contact lenses require less intensive care than specialty contact lenses, given their frequent replacement schedules.
Cons
For patients with severe corneal irregularity, glasses and soft disposable contact lenses typically will not provide functional acuity due to their inability to correct photic phenomena caused by higher-order aberrations (eg, glare, ghosting, and starbursts).
No. 2: Specialty Contact Lenses
Specialty contact lenses can be life-changing for patients with keratoconus. These modalities can create the tear prism necessary to mask the irregular anterior corneal surface, thereby eliminating or significantly reducing the negative visual impact of higher-order aberrations induced by ectatic corneal diseases.
Pros
Unlike other optical tools and most surgical interventions, specialty contact lenses can both neutralize higher-order aberrations related to anterior corneal irregularity and correct lower-order aberrations inherent to the eyes. Specialty contact lenses can thus instantly improve visual function, and they are arguably the best option for maximizing visual quality in most, if not all, patients with keratoconus.
Cons
Depending on the patient’s insurance coverage, the cost of these medically necessary devices can be challenging. In addition, a learning curve for device handling and care is required, varying by lens type. For patients with manual dexterity challenges, deep set eyes, or strong blink reflexes, inserting and removing scleral contact lenses in particular may be an arduous and even frustrating process.
No. 3: Intrastromal Corneal Ring Segments
Intrastromal corneal ring segments, or ICRSs (ie, Intacs; CorneaGen), are plastic corneal inserts shaped like half-moons or arcs. These PMMA segments are surgically implanted into the deep stroma, usually through channels created by a femtosecond laser. ICRS positioning is customized to patients’ own topographic presentations, and the goal of treatment is to flatten the corneal apex and vicinity. As such, ICRSs can also be effective for either keratoconus or postsurgical ectasia. A newly emerging clinical trend is to insert one segment near the area of the inferior cone. This single-segment strategy tends to result in maximal net amount of corneal regularization because it diverts the ICRS’ topographic flattening action toward the cone area while avoiding further flattening the already flatter superior cornea. Thus, this form of treatment may be most optically beneficial for ectasia that has a topographic pattern resembling pellucid marginal degeneration.
Pros
One benefit of ICRSs is that the devices can be implanted either as a standalone procedure or in combination with CXL. Although CXL offers benefits of corneal stabilization, the corneal reshaping effects of ICRS may enhance visual acuity and visual quality with glasses and soft contact lenses (see Quick Tip).
Another perceived benefit of ICRSs is that corneal flattening is achieved through a treatment strategy of addition, rather than the tissue removal involved in PRK (see below).
Cons
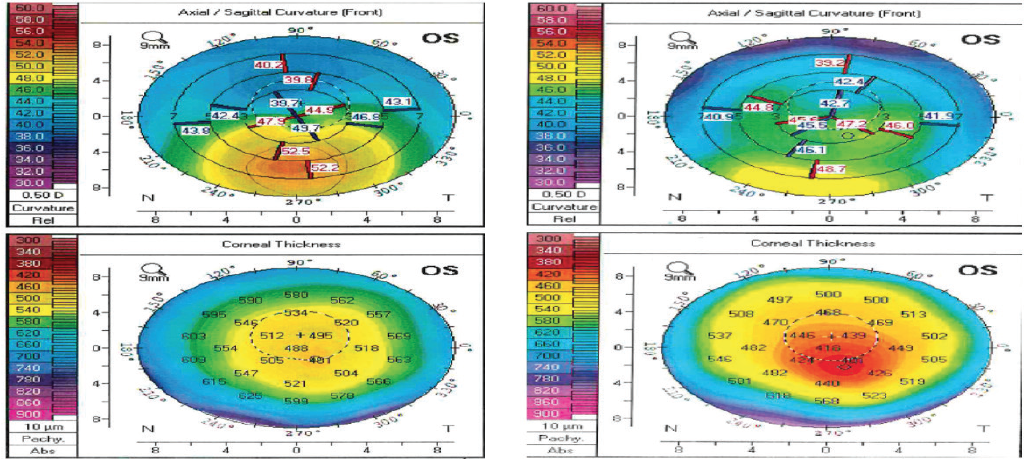
In many cases, an ICRS can reduce corneal protrusion, but the magnitude of the flattening effect is often unpredictable. Moreover, implanting synthetic material into deep stroma carries risks, the biggest of which is stromal melting (Figure 1).5 The most common cause of ICRS-induced corneal melts is ring migration toward the incision site, but thin corneas preoperatively, eye rubbing, ectatic progression, corneal trauma, and corneal infiltrates or ulcers are all predisposing factors.5 Figure 1. Valley in the slit-lamp beam signifying inferior ICRS melt nearly 1 year after implantation. The risk of corneal melts warrants consideration, particularly for young patients. ICRSs are likely best suited to patients for whom contact lenses have failed and who are looking for a treatment method to defer the need for a corneal transplant. In addition, Kanellopoulos and colleagues are studying a combination of porcine xenograft ICRSs with CXL, which has shown promise of corneal flattening in early results.6 If proven viable, this new ICRS implantation strategy may reduce the risks of complications such as stromal melt and corneal erosion. No. 4: Topography-Guided PRK Topography-guided PRK (TG-PRK) incorporates unique shape data from each patient’s cornea into a laser ablation profile. The primary goal of treatment is to regularize the anterior corneal shape with the minimal amount of tissue ablation. Although not FDA approved for use in irregular corneas, some surgeons are offering this technology as an off-label treatment for irregular corneas. With TG-PRK, surgeons can focus treatment on particular areas of the cornea, titrating the resultant corneal flattening. Particularly for keratoconus patients after CXL, this means focalized flattening at the cone apex while minimizing ablation centrally and superiorly (Figure 2). Figure 2. This patient’s visual acuity was 20/70 before he underwent TG-PRK in the left eye. Preoperative anterior segment tomography (Pentacam, Oculus) results are shown at left. At 1 month postoperative the eye was very dry with superficial punctate keratitis, but UCVA was 20/60. Tomography images at 6 months post–TG-PRK are shown at right. There is evidence of 4.00 D of inferior flattening, whereas superiorly there is steepening resulting from peripheral laser treatment. Pros TG-PRK can be combined with CXL during the same treatment session or at separate times in a staged treatment process. With TG-PRK, eye care providers can offer refractive surgery to patients who have keratoconus in order to regularize their corneal profile and thereby improve BCVA and perhaps UCVA. This is generally an exciting prospect for patients. Discussion of TG-PRK can also augment efforts to educate patients about the goal of CXL (ie, to maintain rather than drastically improve BCVA). Cons Protocols and large volumes of patients have not been well studied in the United States. Patient education is essential because the results of TG-PRK are variable after CXL. The key to maximum success with refractive and optical technologies in patients with keratoconus is first to stabilize their ectasia with CXL. The new paradigm for this patient population should be early diagnosis followed by early CXL and finally refractive or optical rehabilitation. A recent study provided evidence in support of this approach. In a retrospective analysis of the effectiveness of CXL for treating keratoconic eyes, those with a baseline Kmax value that was greater than or equal to 58.00 D had a much higher risk of keratoconic progression than has been previously reported.7 Although advanced disease severity does not necessarily exclude CXL as a valid intervention,8 this study does highlight the abundance in clinical benefits when patients are provided early access to CXL. 1. Ferdi AC, Nguyen V, Gore DM, Allen BD, Rozema JJ, Watson SL. Keratoconus natural progression: a systematic review and meta-analysis of 11 529 eyes. Ophthalmology. 2019;126(7):935-945. 2. Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1986;101(3):267-273. 3. Belin MW, Lim L, Rajpal RK, Hafezi F, Gomes JAP, Cochener B. Corneal cross-linking: current USA status: report from the Cornea Society. Cornea. 2018;37(10):1218-1225. 4. Hersh PS, Stulting RD, Muller D, Durrie DS, Rajpal RK; United States Crosslinking Study Group. United States multicenter clinical trial of corneal collagen crosslinking for keratoconus treatment. Ophthalmology. 2017;124(9):1259-1270. 5. Jarade E, Issa M, Chanbour W, Warhekar P. Biologic stromal ring to manage stromal melting after intrastromal corneal ring segment implantation. J Cataract Refract Surg. 2019;45(9):1222-1225. 6. Kanellopoulos AJ, Vingopoulos F. Combining porcine xenograft intra-corneal ring segments and CXL: a novel technique. Clin Ophthalmol. 2019;13:2521-2525. 7. Kuechler SJ, Tappeiner C, Epstein D, Frueh BE. Keratoconus progression after corneal cross-linking in eyes with preoperative maximum keratometry values of 58 diopters and steeper. Cornea. 2018;37(11):1444-1448. 8. Ivarsen A, Hjortdal J. Collagen cross-linking for advanced progressive keratoconus. Cornea. 2013;32(7):903-906.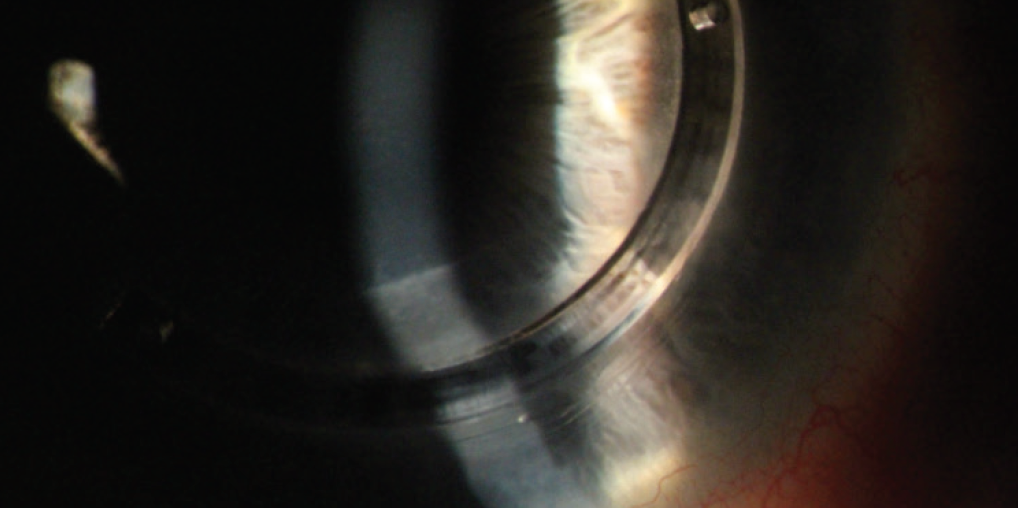
DIAGNOSE EARLY, STABILIZE ECTASIA, AND REHABILITATE



