Three values that are continuously rising among the US population are the mean age, the number of cataract surgeries performed per year, and the number of patients diagnosed with glaucoma per year.1 In 2017, nearly 4 million cataract surgeries were performed in the United States, up from 3.6 million in 2015.2
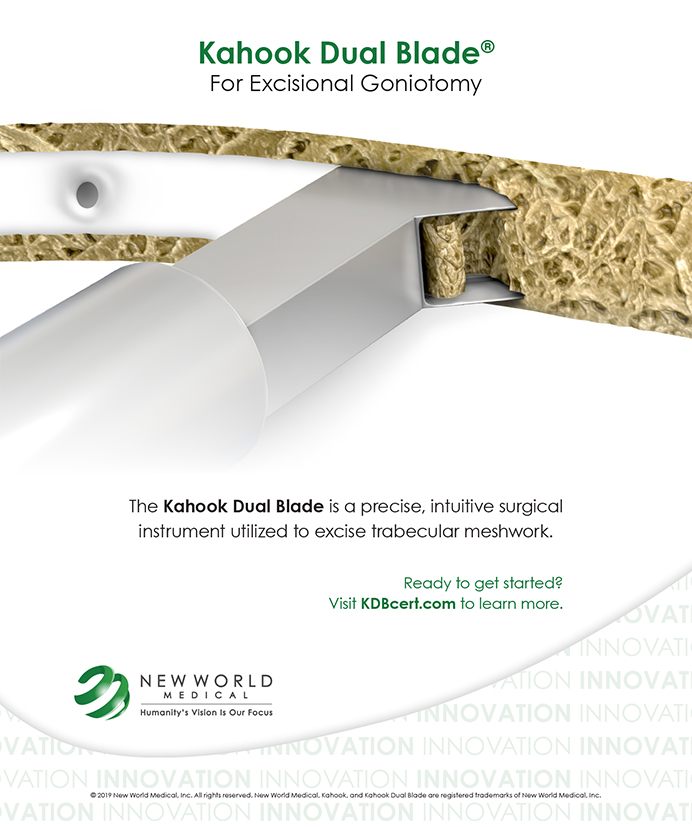
Cataract surgery alone can be considered a treatment for glaucoma. Multiple studies have shown that removing the thickening cystic lens and replacing it with a thinner IOL can lower IOP by 2 mm Hg to 5 mm Hg.3,4 Microinvasive glaucoma surgery (MIGS) has been a powerful addition to the options for patients with comorbid cataracts and glaucoma. When we speak to our patients with glaucoma about cataract surgery, it is an excellent time to recommend a concurrent MIGS procedure.
BEGINNING COLLABORATION
Collaborating with a surgeon or surgical center starts with building a relationship around trust and communication. For patients with concomitant cataract and glaucoma, if a combined surgical procedure is desired, referring to an ophthalmologist who performs MIGS or other glaucoma procedures is the first step in the process.
The second step is communicating with the ophthalmologist via a high-quality referral letter. Often, the patients you refer have been seeing you as their primary optometrist for many years, whereas the ophthalmologist may have only a 15-minute consultation with the patient. A letter outlining a brief patient history and pertinent personality traits can be helpful to provide to the ophthalmologist. For cataract patients, notes on the patient’s visual goals and postoperative expectations can help drive satisfaction. For glaucoma patients, attaching visual fields and OCTs (although many surgical centers may repeat them), noting maximum IOP history, and discussing recent glaucoma stability can all be beneficial for the ophthalmologist.
As a final step, the optometrist should also let the ophthalmologist know about his or her aspirations to comanage the patient.
PREOPERATIVE CARE
Optometrists should strive to be the frontline diagnosticians and detectives for patients with both cataract and glaucoma. When a patient with glaucoma has visual concerns due to cataract, the optometrist should make the referral for cataract surgery with the consideration of adding a glaucoma procedure. When we educate patients about cataracts, with or without glaucoma surgery, all optometrists should inform patients about the following two things, at minimum.
First, let patients know that the surgeon will present vision correction options that can be performed at the time of cataract surgery. Second, let your glaucoma patients know that they may be candidates for a concurrent MIGS procedure that could lower their risk of glaucoma progression and potentially make them less dependent on glaucoma medications.
Until the patient undergoes surgical evaluation, continuing current topical glaucoma medications is preferred, both to prevent glaucomatous damage and to allow the surgeon to use the full toolbox of MIGS procedures from an insurance standpoint.
POSTOPERATIVE CARE
Optometrists are well equipped for comanagement of many MIGS procedures. Most MIGS procedures do not complicate comanagement any more than traditional cataract surgery comanagement, which optometrists are already handling. This is not to say that different surgical procedures do not have different depths of postoperative management and possible comorbidities.
Each ophthalmologist mayhave a different comanagement paradigm. Gonioscopy is one key skill differentiator when it comes to comanaging patients with combined cataract-MIGS procedures that are angle-based (trabecular meshwork/Schlemm canal). The area that is stented or operated on cannot be directly assessed without a gonioscopy mirror. Performing gonioscopy once postoperatively on these patients is sufficient, unless there are suspicious or unexpected events in the postoperative period.
KEY CONSIDERATIONS IN COMBINED CATARACT-MIGS PROCEDURES
IOP Spikes
On postoperative day 1, vision and IOP can be quite variable, as is the case with any cataract surgery. Corneal edema can lead to decreased vision from endothelial disruption and/or elevated IOP. Sadly, even after a MIGS procedure, IOP spikes from retained viscoelastic material (1 to 2 days postoperative) or steroids (4 to 30 days postoperative) can still occur. In the first 48 hours, IOP spikes can be controlled by burping the wound to remove aqueous and ophthalmic viscosurgical device material and adding a topical aqueous suppressant.
At 1 week and, more commonly, 2 to 4 weeks postoperative, if an IOP spike is thought to be steroid-induced, the comanaging doctor can speed up the taper of the steroid to aid in normalizing IOP. In surgical cases in which intracameral injections are used for postoperative healing, understanding the duration of the medicine in the eye and dosing topical glaucoma medications accordingly can help to manage steroid-induced IOP increases.
Iatrogenic Microhyphema
Angle-based MIGS procedures and those using supraciliary devices involve the stenting, cutting, ablating, or dilating of tissue, which can lead to reflux and iatrogenic hyphemas. In my experience with MIGS procedures, microhyphemas are present on postoperative day 1 in 0% to 15% of cases, depending on the specific procedure. These hyphemas are not typically visually significant and are almost all self-resolving by 1 to 2 weeks postoperative. The best treatment in this situation is patient counseling.
Hypotony
A benefit of MIGS procedures is that they minimize the risk of postoperative hypotony compared with incisional glaucoma procedures. In angle-based procedures, where episcleral venous pressure is present, the risk of hypotony should be close to zero. The risk of hypotony is greater with supraciliary and subconjunctival MIGS procedures but is still decreased in comparison with incisional filtering procedures (tube shunts and trabeculectomies). If you see a patient with immediate postoperative hypotony with a formed anterior chamber, a call to the ophthalmologist who performed the procedure is warranted, at minimum. Patients with chronic hypotony should be referred back to the operating surgeon.
Other Considerations
Patients are commonly seen at 1 week and 1 month postoperative. The most common comanagement conundrum for patients undergoing cataract-MIGS surgery is how to titrate topical glaucoma medications postoperatively. Confidence will grow with experience in managing these patients, but a general rule of thumb with angle-based MIGS is to be cautious with removing glaucoma medications in the early postoperative period. At 6 to 8 weeks postoperative, when the steroid taper is complete, it is safe to decrease medications with close monitoring of IOP as medications are removed.
It is important to inform patients that a medication may be removed for a period of time but added back to the regimen if IOP does not respond as anticipated. With supraciliary and, even more important, subconjunctival procedures, removing medications can aid in forcing flow through the surgical stent. In the event of numerical hypotony after supraciliary or subconjunctival procedures, all topical glaucoma medications should be stopped until the IOP elevates. Cycloplegia to relax the anatomy can also be useful in the presence of hypotony.
As in routine cataract surgery, refraction should be performed 2 to 4 weeks postoperatively. At 3 to 6 months after the cataract-MIGS procedure, new baseline visual fields and OCTs should be obtained and a new target IOP determined.
A CONTINUING NEED
Unfortunately, cataract surgery plus MIGS will not reverse your patient’s existing glaucomatous damage, nor will it provide a permanent cure for glaucoma. However, the combined procedures can be effective for patients.
In the subset of MIGS procedures approved to be done in conjunction with cataract surgery, the safety aspiration of “as safe as cataract surgery alone” can almost be thought of as a “free lunch” for patients with concomitant cataract and glaucoma. Topical glaucoma medications are highly effective, but I believe that if you asked glaucoma patients whether they would like to decrease their medication burden, they would almost universally say yes. Remember, at the time of cataract surgery, resistance (insurance) is least and safety (already operating inside the eye) is highest for the majority of MIGS procedures.
By my estimation, based on survey and US government workforce data, optometrists are comanaging less than 25% of the cataract surgeries performed today in the United States. By embracing the comanagement of these patients, optometrists can leverage continuity of care and allow surgeons more flexibility in their schedules to provide surgery for the patients who need it.
Having a foundational knowledge of the three MIGS outflow pathways (trabecular meshwork/Schlemm canal, supraciliary, and subconjunctival) can help you to provide preoperative education and set appropriate expectations for each individual patient.
Optometry’s opportunity to collaborate in pre- and postoperative care for combined cataract and glaucoma surgery will continue to rise along with the aging of the population, the number of cataract surgeries being performed, and the prevalence of glaucoma.
- Goes F. The future of cataract surgery. Ophthalmology Times. July 10, 2017. ophthalmologytimes.com/ote-articles/future-cataract-surgery. Accessed February 21, 2019.
- Lindstrom RL. Thoughts on cataract surgery: 2015. Review of Ophthalmology. March 9, 2015. reviewofophthalmology.com/article/thoughts-on–cataract-surgery-2015. Accessed February 21, 2019.
- Samuelson TW, Katz LJ, Wells JM, Duh YJ, Giamporcaro JE, US iStent Study Group. Randomized evaluation of the trabecular micro-bypass stent with phacoemulsification in patients with glaucoma and cataract. Ophthalmology. 2011;118(3):459-467.
- Mansberger SL, Gordon MO, Jampel H, et al. Reduction in intraocular pressure after cataract extraction: the ocular hypertension treatment study. Ophthalmology. 2012;119(9):1826-1831.