Cataract surgery has become a refractive procedure, which means that ophthalmologists must address astigmatism to achieve satisfactory results. More than 0.50 D of residual astigmatism is visually significant and can result in ghosting and shadows.1
Before considering astigmatic correction, I perform a qualitative assessment of the corneal surface using topography and a slit-lamp examination. Does the patient have irregular astigmatism, keratoconus, or subtle corneal pathology such as epithelial basement membrane dystrophy? Once I am sure the patient has true corneal astigmatism, I review results from two topographers that can measure anterior and posterior astigmatism as well as perform optical biometry to make sure the magnitude and meridian match among devices (within 0.50 D and 10º, respectively). If there is a big difference between the biometer and the topographers, for example, I consider treating the astigmatism postoperatively.
When picking toricity and the alignment meridian, I use the Baylor Nomogram as well as the IOL manufacturer’s online calculator. The data I enter are an average of the measurements obtained with the two topographers and the optical biometer I used, typically the Galilei Dual Scheimpflug Analyzer (Ziemer Ophthalmic Systems), Cassini (i-Optics), and IOLMaster 700 (Carl Zeiss Meditec). Surgeons without all of these tools can still use toric IOLs effectively. Placing a toric IOL based on consistent astigmatism measurements between a topographer and biometer using manual markings can produce excellent refractive outcomes.
I recommend toric IOLs for patients with as little as 0.80 D of against-the-rule (ATR) astigmatism, especially if they have a high amount of posterior corneal astigmatism. I also favor a toric IOL if the patient has 1.00 D or more of with-the-rule (WTR) astigmatism. I use a 2.4-mm incision, which results in minimal surgically induced astigmatism.2 Patients who have chosen a multifocal or extended depth of focus IOL should also have their astigmatism corrected to decrease the risk of blurry vision, glare, and halos.
In the United States, the main toric platforms are the Tecnis Toric IOL (ZCT line, Johnson & Johnson Vision [J&J Vision]) and the AcrySof IQ Toric IOL (SN6AT line, Alcon). Combining presbyopic and astigmatic correction are the Tecnis Symfony Toric IOL (J&J Vision), the AcrySof IQ Restor +2.5 D Multifocal Toric IOL with Activefocus optical design (Alcon), the AcrySof IQ Restor +3.0 D Multifocal Toric IOL (Alcon), and the Trulign Toric IOL (Bausch + Lomb). I have experience with the platforms from J&J Vision and Alcon, and both are excellent for correcting astigmatism. Data show that Alcon’s platform rotates less than J&J Vision’s.3,4
CASE EXAMPLE
A 66-year-old man presented with decreased vision, glare, and halos that were affecting his ability to drive at night. A slit-lamp examination showed a 2+ nuclear sclerotic cataract, but the rest of the anterior segment and posterior segment examination was normal. There were no signs of dry eye disease. Placido ring topography showed crisp rings and no sign of epitheliopathy.
The patient had significant astigmatism on manifest refraction, both topography devices, and the biometer, and it was similar in magnitude and meridian on all devices (Figures 1 and 2). Using the magnitude and meridian of astigmatism from the Lenstar (Lenstar), I entered preoperative data into the Baylor nomogram and the Alcon online toric calculator, which incorporates the Barrett calculator. Both nomograms recommended a 17.00 D model SN6AT8 AcrySof IQ Toric IOL (Alcon) to minimize ATR astigmatism without flipping the axis. Given the ATR shift in astigmatism with age, I left the patient with a little WTR astigmatism.
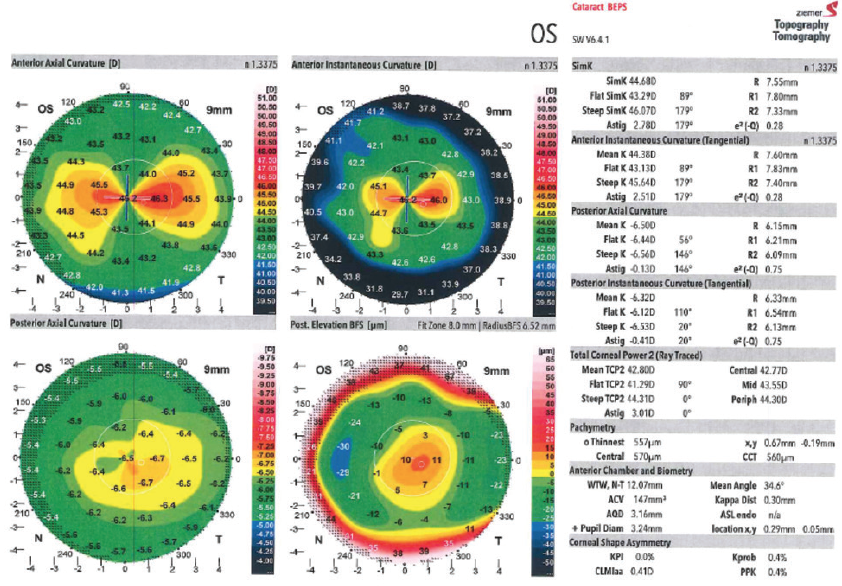
Figure 1. The Galilei Dual Scheimpflug Analyzer showed the magnitude and meridian of astigmatism in the patient’s left eye.
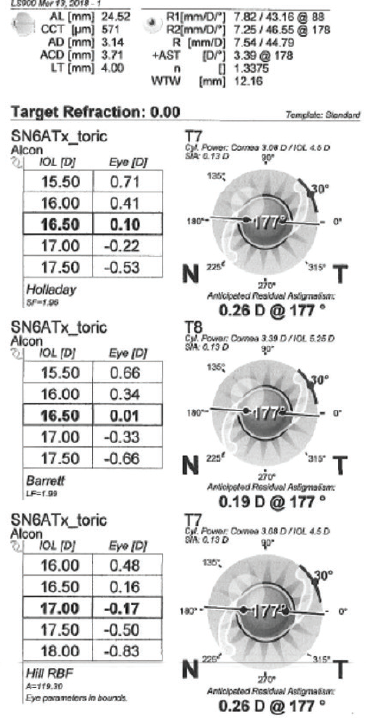
Figure 2. The Lenstar biometer showed the magnitude and meridian of astigmatism in the patient’s left eye.
In the preoperative area, I manually marked the 3-, 6-, and 9-o’clock axes on the eye. Next, I used the Catalys Precision Laser System (J&J Vision) to place two 10º intrastromal marks at the intended meridian, create the anterior capsulotomy, and soften the nucleus.
In the OR, after removing the cataract and cortex and filling the bag with an OVD, I performed intraoperative aberrometry (ORA System, Alcon), which confirmed the chosen toric IOL and axis. I implanted the IOL and oriented it to the intended axis with bimanual irrigation and aspiration.
Three weeks after surgery, the patient’s UCVA measured 20/20 with a manifest refraction of -0.50 D and no residual astigmatism. He was very happy with the result.
- Villegas EA, Alcón E, Artal P. Minimum amount of astigmatism that should be corrected. J Cataract Refract Surg. 2014;40(1):13-19.
- Montes de Oca I, Khandelwal SS, Al-Mohtaseb Z, et al. Long-term surgically induced astigmatism after cataract surgery. Paper presented at: ASCRS/ASOA Congress & Symposium; May 6-10, 2016; New Orleans, LA
- Potvin R, Kramer BA, Hardten DR, Berdahl JP. Toric intraocular lens orientation and residual refractive astigmatism: an analysis. Clin Ophthalmol. 2016;10:1829-1836.
- Lee BS, Chang DF. Comparison of the rotational stability of two toric intraocular lenses in 1273 consecutive eyes [published online ahead of print March 12, 2018]. Ophthalmology. doi:10.1016/j.ophtha.2018.02.012.
- Ho JD, Liou SW, Tsai RJ, Tsai CY. Effects of aging on anterior and posterior corneal astigmatism. Cornea. 2010;29(6):632-637.
- Smith EM Jr, Talamo JH. Cyclotorsion in the seated and supine patient. J Cataract Refract Surg. 1995;21(4):402-403.



