By definition, calculating for a toric IOL requires selecting a spherical power, cylindrical power, and axis. All patients in our office receive three preoperative astigmatism measurements: auto keratometer, IOLMaster 700 (Carl Zeiss Meditec), and iTrace (Tracey Technologies). The iTrace gives a best-fit keratometry (K) reading cumulatively through the central 3 mm that I use instead of its simulated K readings. It is critical that the patient’s head be level, even if it is habitually tilted, and the studies should be performed on a pristine cornea. Patients are asked to stop wearing soft contact lenses 2 weeks prior to their visit and rigid gas permeable lenses 3 weeks before their appointment—longer if necessary for their corneal topography to become regular.
The ideal candidate for toric correction has regular astigmatism, with agreement among the three K measurements. Fortunately, most individuals fit this description. Simply picking the toric power based on this number, however, can lead to unsatisfactory results.
It is important to keep the axis of the correction in mind, undercorrecting with-the-rule cylinder and overcorrecting against-the-rule cylinder. As reported by Koch et al, the posterior cornea causes against-the-rule cylinder that is not captured well by most devices.1-3 Furthermore, IOLs with high spherical powers have a greater toric effect, even if their toricity is identical.4-7 That means that a +28.00 D SA6AT4 AcrySof IQ Toric IOL (Alcon) will correct more astigmatism than a +8.00 D SA6AT4 lens. Similarly, the ratio between the toric power at the IOL plane and the corneal plane depends on the IOL’s position.
I do not use a manufacturer’s online calculator, but these tools have improved and are excellent because most take IOL power and posterior corneal astigmatism into account.8-10 Another option now available is the Barrett Toric Formula. It may be accessed through a link in the “Online Tools” area of the American Society of Cataract and Refractive Surgery’s website (www.ascrs.org) or the Asia-Pacific Association of Cataract & Refractive Surgeons’ website (www.apacrs.org). I use the HofferQ, Holladay 1, SRK/T, Holladay 2, Haigis, and Barrett formulas in combination to choose the spherical power and then calculate the cylindrical power separately. I utilize intraoperative aberrometry to fine-tune both the IOL’s spherical power and the axis, but I rarely change the cylindrical power unless I am using aberrometry to help decide between two powers. Using a digital marking system has improved the accuracy of my toric IOL placement and reduced the time I spend on aberrometry adjustments, but with careful marking and technique, surgeons can achieve fantastic results with manual marking alone.
CASE EXAMPLE NO. 1
The patient had undergone cataract surgery with a multifocal IOL in her right eye 10 years earlier. Her habitual glasses prescription in her left eye was -2.75 D sphere, but she reported progressive worsening of her vision and was referred for cataract surgery. Her BCVA was 20/300 with a refraction of -4.00 +5.50 × 95º, and she had a 3+ nuclear cataract. The slit-lamp examination showed nasal Salzmann nodules in her left eye.
I regularly see patients with unrecognized Salzmann nodules. Ideally, nodules that are central or cause significant irregularity should be addressed before cataract surgery. Simply implanting a T9 AcrySof IOL or a ZCT600 Tecnis Toric IOL (Johnson & Johnson Vision) might seem tempting because the Ks were so consistent (keratometer 5.75 D @ 92º; IOLMaster 5.78 D @ 93º; topographer 5.40 D @ 92º). It is better to reduce the cylinder and make the cornea more regular, however, so I performed a superficial keratectomy and removed the Salzmann nodules first. The astigmatism still was not totally symmetric, but it was consistent and much lower in magnitude (keratometer 2.12 D @ 84º; IOLMaster 2.18 D @ 92º; topographer 2.47 D @ 85º). The IOL power changed by more than 3.00 D (Figure 1). Because the astigmatism was with the rule, I implanted an AcrySof SN6AT5 lens and aimed for -1.50 D. The patient achieved a visual acuity of 20/20+2 with -1.50 D sphere.
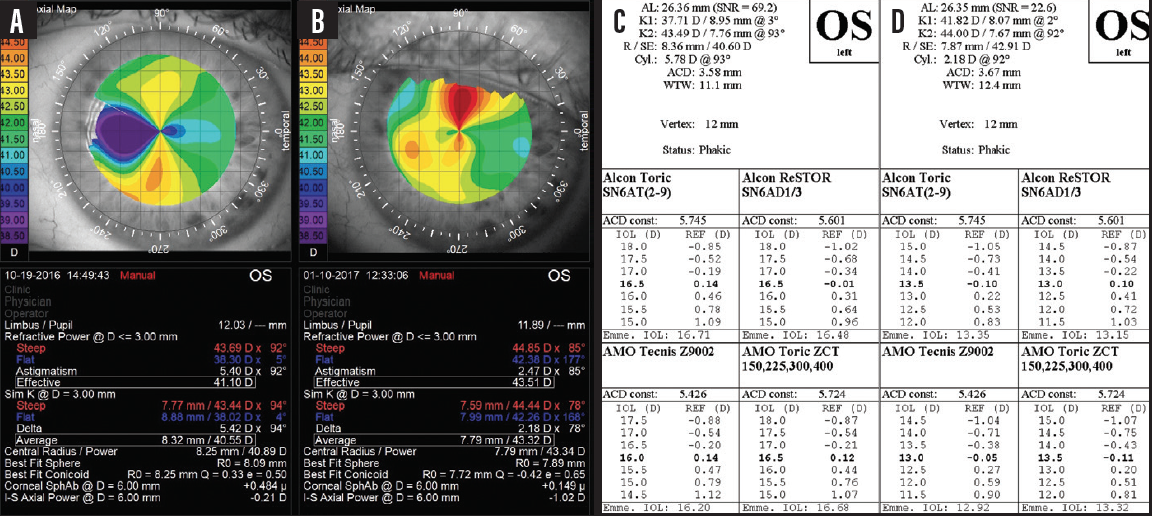
Figure 1. The difference in topography before (A, C) nodule removal and 8 weeks later (B, D).
CASE EXAMPLE No. 2
The patient had a history of bilateral LASIK and presented with a decline in vision from cataract. She desired intermediate myopia in her left eye, which she had had after LASIK.
The refractive power measurement, which sums up the central 3 mm of the cornea, showed astigmatism of 1.83 D @ 123º. There was definite asymmetry, however, and the patient had significant coma, as evident in the aberrations displayed in the lower left corner of Figure 2. Her Ks were 1.63 D @ 102º, whereas her IOLMaster Ks were 1.28 D @ 113º. A repeat IOLMaster measurement was 1.87 D @ 117º.
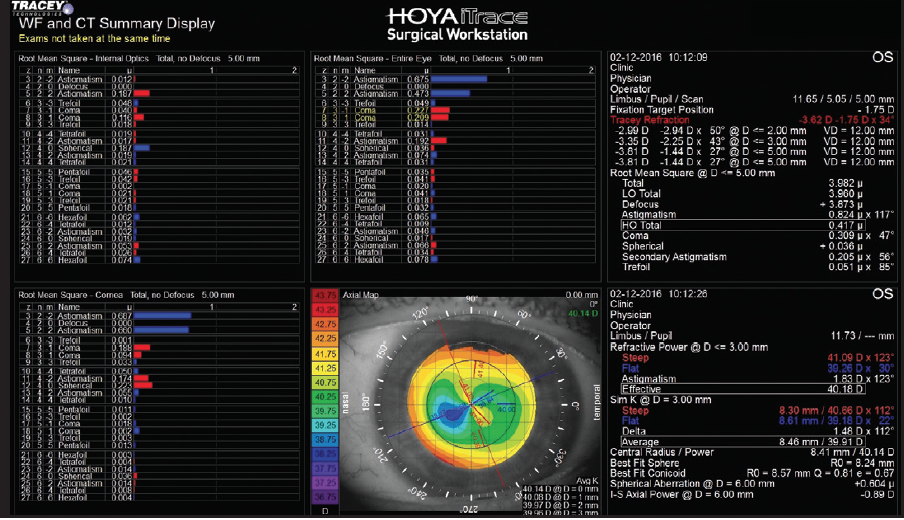
Figure 2. The patient shows typical post-LASIK changes, which can make correcting astigmatism more challenging.
Irregular astigmatism and mildly inconsistent measurements are common among post-LASIK patients. Having this patient use artificial tears frequently and repeating the biometry helped because the subsequent IOLMaster Ks were consistent with the topography measurements. In this situation, the auto Ks were the outlier. I think that is because that instrument was measuring farthest from the center of the cornea. The more central portion of the topography was consistent with the 123º axis, and the more peripheral cornea was consistent with the 102º axis from the keratometer. After considering all of the measurements together, I implanted a ZCT225 (Johnson & Johnson Vision) at 123º, and the patient achieved a visual acuity of 20/20 with -1.25 D sphere.
- Koch DD, Ali SF, Weikert MP, et al. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38(12):2080-2087.
- Koch DD, Jenkins RB, Weikert MP, et al. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. J Cataract Refract Surg. 2013;39(12):1803-1809.
- Koch DD. The enigmatic cornea and intraocular lens calculations: The LXXIII Edward Jackson Memorial Lecture. Am J Ophthalmol. 2016;171:xv-xxx.
- Goggin M, Moore S, Esterman A. Toric intraocular lens outcome using the manufacturer’s prediction of corneal plane equivalent intraocular lens cylinder power. Arch Ophthalmol. 2011;129(8):1004-1008.
- Goggin M, Moore S, Esterman A. Outcome of toric intraocular lens implantation after adjusting for anterior chamber depth and intraocular lens sphere equivalent power effects. Arch Ophthalmol. 2011;129(8):998-1003.
- Savini G, Hoffer KJ, Ducoli P. A new slant on toric intraocular lens power calculation. J Refract Surg. 2013;29(5):348-354.
- Eom Y, Kang SY, Song JS, et al. Effect of effective lens position on cylinder power of toric intraocular lenses. Can J Ophthalmol. 2015;50(1):26-32.
- Abulafia A, Barrett GD, Kleinmann G, et al. Prediction of refractive outcomes with toric intraocular lens implantation. J Cataract Refract Surg. 2015;41(5):936-944.
- Park HJ, Lee H, Woo YJ, et al. Comparison of the astigmatic power of toric intraocular lenses using three toric calculators. Yonsei Med J. 2015;56(4):1097-1105.
- Ferreira TB, Ribeiro P, Ribeiro FJ, O’Neill JG. Comparison of astigmatic prediction errors associated with new calculation methods for toric intraocular lenses. J Cataract Refract Surg. 2017;43(3):340-347.