West Virginia authorized optometrists to include the treatment of glaucoma in their scope of practice in 1978; since then, 49 states and the District of Columbia have allowed ODs to provide glaucoma treatment. Pending legislation in Massachusetts, if signed into law, would allow every optometrist in the United States to manage glaucoma.
But glaucoma drops are only part of the solution in contemporary glaucoma management. Now that glaucoma is no longer a disease managed only by pharmacologic solutions, many patients will turn to their optometrists for answers to questions about the nuances of such surgeries.
INCREASING ROLE OF SURGERY
Historically, treating a newly diagnosed patient with open-angle glaucoma (OAG) consisted of setting a target intraocular pressure (IOP) and prescribing an appropriate eye drop to achieve that target. This plan, however, comes with problems: ever-increasing costs of medications, constant counseling on the need for daily compliance, and any number of side effects. Prior to recent innovations, surgical intervention was traditionally regarded as treatment only for advanced or refractory cases that did not respond sufficiently to medical and laser options.
Optometrists are poised to fulfill a crucial role in managing the care of their patients with glaucoma. The new normal often starts with giving the patient options other than topical agents as first or second-line treatment.
In our practice, we educate newly diagnosed OAG patients about all of their treatment options and work with them to choose the most appropriate course. We typically educate patients on the risks and benefits of starting with either selective laser trabeculoplasty or topical therapy, knowing that, according to the Glaucoma Laser Trial, either treatment would be an equally acceptable choice.1 We find that more than 90% of our patients choose laser therapy in lieu of drops, citing the aforementioned cost and compliance issues.
COMBINED SURGERY
Patients with glaucoma and cataract present a unique opportunity to address IOP without medication. If a cataract is visually significant and affecting a patient’s activities of daily living, we recommend the option of phacoemulsification on its own or combined with a minimally invasive glaucoma surgery (MIGS) procedure.
MIGS devices have transformed the treatment protocol for all glaucoma patients because of their ability to achieve consistent IOP control independent of patient compliance while lowering the incidence of both side effects and surgical complications (Table).
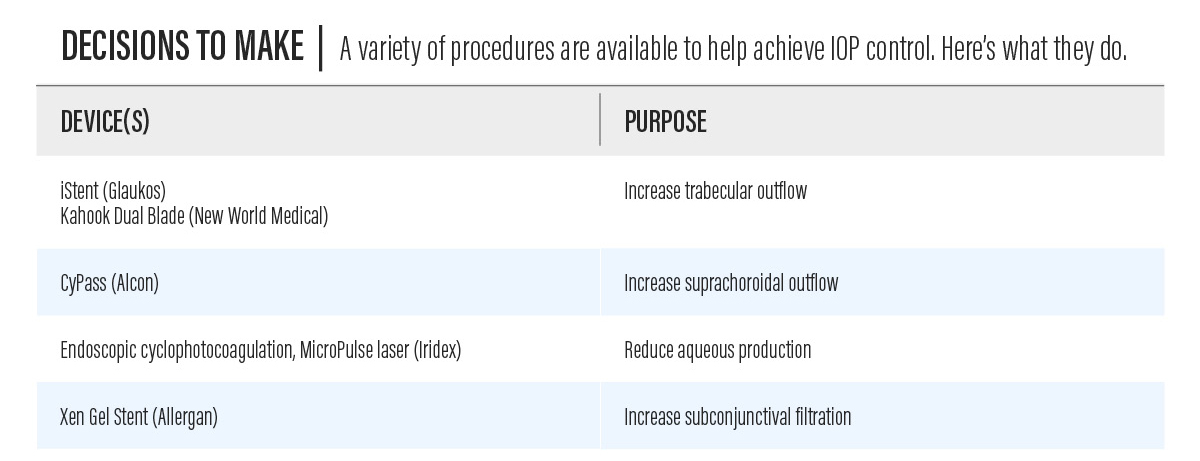
Table. A summary of MIGS devices and their purposes.
For glaucoma patients who are ready for cataract surgery, we suggest phacoemulsification combined with MIGS. A patient, for example, may have cataract surgery combined with insertion of an »iStent device (Glaukos) to reduce resistance to trabecular outflow. If more significant IOP reduction is required, we may suggest combining the iStent with endoscopic cyclophotocoagulation (»ECP; Endo Optiks) to simultaneously reduce aqueous production.
We also find that the »Kahook Dual Blade (New World Medical) is a great way to reduce trabecular resistance without implanting a stent. This specially designed handpiece for minimally invasive goniotomy strips a small section of the trabecular meshwork to increase outflow.
Another effective MIGS device that can be combined with cataract surgery is the »CyPass Micro-Stent (Alcon). This device, implanted posterior to the scleral spur between the sclera and ciliary body, increases aqueous outflow by directly communicating with the suprachoroidal space to lower IOP. In addition, the »Xen Gel Stent (Allergan) is a device implanted via an ab interno approach to create a channel for aqueous to filter into the subconjunctival space.
Postoperative management of patients who have undergone MIGS procedures is generally similar to management of patients who have undergone cataract surgery alone. Following the customary 1-day post op visit, we monitor the patient in 1 to 2 weeks to check inflammation, and then again in 4 to 6 weeks to assess postoperative IOP. Afterward, patients can often enjoy freedom from (or less dependence on) topical therapy. Further, in our experience, these procedures carry much lower risk of hypotony, choroidal effusion, or decreased vision compared with traditional incisional filtering surgery.
A NEW DAY FOR GLAUCOMA
As the patient’s primary eye care provider, the optometrist must navigate advances in technology, educate patients on treatment options, and regularly communicate with the comanaging surgeon to coordinate appropriate care. Gone are the days when we would diagnose a patient, prescribe an eye drop, and monitor IOP endlessly. It should be noted, however, that many patients—including those who have had MIGS or other surgeries—still require medical therapy to control their disease.
Optometrists are in the driver’s seat when a patient’s treatment plan is set in motion. They monitor pressure, visual fields, and imaging. If IOP becomes poorly controlled or progression of disease is suspected, consultation with the comanaging physician is advised. When a plan to stabilize the patient is decided upon by the optometrist and the ophthalmologist, the optometrist returns to managing the patient.
This seamless comanagement of glaucoma patients can be conducted inside an integrated practice or between optometrists (whether commercial or independent) and their ophthalmology colleagues. In the latter case, an optometrist may monitor all of the patient’s testing and share it with the consulting MD, eliminating redundant health care costs. This convenience for patients keeps them happy and reduces their overall time spent in doctors’ offices.
- The glaucoma laser trial (GLT): Results of argon laser trabeculoplasty versus topical medicines. Ophthalmology. 1990;97(11):1403–1413.