LASIK and PRK are the two most commonly performed corneal refractive surgical procedures in the world. After the clinician confirms via preoperative screening that a patient is an appropriate candidate for laser vision correction, the clinician is then equipped to make a surgical recommendation. If the clinician is an optometrist or an ophthalmologist who will not perform the surgery, this suggestion will be reviewed by the patient’s surgeon before proceeding. The recommendation is key in refractive surgery, as it sets the stage for the patient’s expectations and postoperative course.
Patients usually prefer LASIK over PRK due to its rapid recovery time, faster visual improvement, and reduced postoperative discomfort compared with the surface procedure. Studies have shown that patients who undergo LASIK achieve faster postoperative visual recovery than patients undergoing other refractive surgical procedures,1,2 although visual acuity is comparable between procedures once it is stable. Like all surgical decision-making, the decision is patient-specific and multifactorial.
STROMAL BED
Often, the primary driver in recommending LASIK or PRK is centered around preserving the biomechanical integrity of the cornea. Normal corneas are at low risk for destabilization. When corneas have borderline features, PRK may be the preferred choice. PRK has a lower risk profile because it involves no LASIK flap creation.3 Therefore, there is a deeper residual stromal bed and lower percentage of altered tissue.
Patients for whom LASIK is appropriate should have a relatively normal corneal thickness (> 500 µm), which will leave a residual stromal bed depth of greater than 300 µm. The patient should also have normal topographic, tomographic, and biomechanical parameters. If the patient has slightly abnormal topographic, tomographic or biomechanics parameters; thin corneas (< 500 µm); or has previously undergone refractive surgery, PRK is often favored over LASIK.3
UNIQUE PRK CONSIDERATIONS
Dense corneal scars can block the plasma pulses from femtosecond lasers, leading to incomplete flap creation. Therefore, in eyes with corneal scarring, either PRK or LASIK with a mechanical microkeratome may be the better choice.
Epithelial dystrophy, such as epithelial basement membrane dystrophy, is an indication for PRK. The surface procedure not only treats the refractive error but also treats the underlying dystrophy, reducing epithelial irregularities and improving quality of vision. Further, it should be noted that, although rare, femtosecond laser use in LASIK flap creation may result in vertical gas breakthrough in patients with epithelial basement membrane dystrophy. Patients with endothelial cell dystrophy may also benefit from PRK rather than LASIK because their endothelial dysfunction may impair flap adherence.
PRK may be recommended for patients who play contact sports or those in the military or police because such patients are more prone to eye trauma that may (however rarely) lead to damage or loss of the LASIK flap.
SCREENING
New refractive surgical screening analyses are useful and evolving, but Placido-disc–based corneal topography is still considered the gold standard for screening. Tomography is also extremely useful (Figure). It allows creation of pachymetry maps and anterior and posterior corneal elevation maps, in addition to providing more advanced screening analysis.
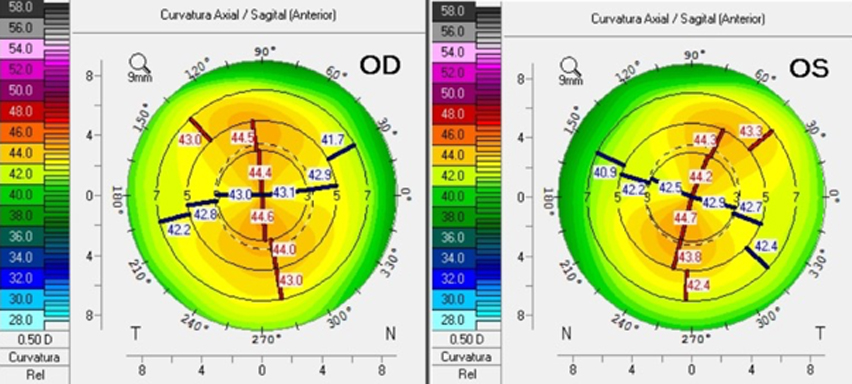
Figure. Corneal tomography of a 25-year-old patient who is a candidate for laser vision correction. The patient has a refraction of -3.75 -0.75 @ 5o OD and -4.00 -1.00 @ 165o OS. Topography shows regular symmetric with the rule astigmatism of 1.4 OD and 1.6 OS.
At our center, we have been evaluating multiple biomechanical devices that are promising, and we routinely use combined tomographic and biomechanical analysis to help determine candidacy for LASIK or PRK. We have also been beta testing commercial finite element modeling, which shows promise.
WEIGHING YOUR OPTIONS
Both LASIK and PRK are safe and effective treatments for ametropia, including astigmatism, and both can result in high levels of patient satisfaction. The choice between the two procedures is patient-dependent, and quality chair time is essential to provide sufficient patient education, set appropriate expectations, and deliver postoperative satisfaction to our patients.
- Hatch BB, Moshirfar M, Ollerton AJ, et al. A prospective, contralateral comparison of photorefractive keratectomy (PRK) versus thin-flap LASIK: assessment of visual function. Clin Ophthalmol. 2011;5:451-457.
- Hashemi H, Miraftab M, Ghaffari R, Asgari S. Femtosecond-assisted LASIK versus PRK: comparison of 6-month visual acuity and quality outcome for high myopia. Eye Contact Lens. 2016;42(6):354-357.
- Santhiago MR, Wilson SE, Hallahan KM, et al. Changes in custom biomechanical variables after femtosecond laser in situ keratomileusis and photorefractive keratectomy for myopia. J Cataract Refract Surg. 2014;40(6):918-928.







