Approximately 86% of all patients with dry eye disease (DED) have meibomian gland dysfunction (MGD) as a primary or contributing component of their condition.1 Studies have indicated that a majority of patients presenting for cataract surgery have MGD2,3 and that the condition is becoming increasingly common, even among children.4 Recognizing and treating MGD need not be complicated. Here are three common scenarios every clinician should be able to identify and manage.
PREOPERATIVE CATARACT PATIENT WITH FLUCTUATING VISION
A 72-year-old man presented for cataract surgery with an interest in spectacle independence. He said his eyes felt fine but noted that his vision was worse at the end of the day and after reading. Examination revealed a 3+ nuclear sclerotic cataract, tear breakup time of 2 to 3 seconds, and MGD with telangiectasia of the lid margins. Initial testing with the »IOLMaster (Carl Zeiss Meditec) recommended a toric IOL for each eye, but biometry cannot be trusted when the tear film quality is poor. An irregular tear film may cause erroneous keratometry readings and suboptimal IOL selection.5
The patient was treated with vectored thermal pulsation therapy (VTP; »LipiFlow, Johnson & Johnson Vision), microblepharoexfoliation (»BlephEx, Rysurg), loteprednol etabonate ophthalmic ointment 0.5% (»Lotemax, Bausch + Lomb) for an immediate antiinflammatory effect, and 50 mg oral doxycycline twice daily.
One month later, the patient’s keratometry readings had changed considerably, and the IOLMaster recommended a lower-powered toric IOL for the left eye and a spherical IOL for the right eye (Table).
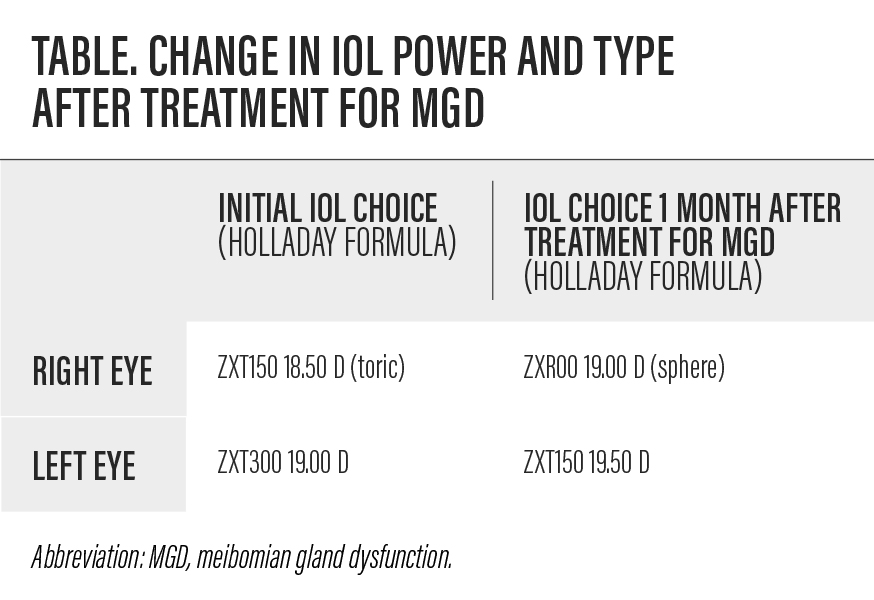
Given the prevalence of MGD in the cataract patient population, clinicians should evaluate the meibomian glands of every preoperative patient whether or not they are symptomatic. Although older patients may not complain of dryness or irritation, vision that fluctuates throughout the day suggests the possibility of MGD. Irregular mires on topography are another warning sign of possible ocular surface disease (Figure).

Figure. Irregular mires are an indication of ocular surface disease. Treatment is warranted before obtaining final biometry, IOL calculations, and other preoperative measurements. Photo credit: Alice Epitropoulos, MD.
PATIENT WITH THICK OR NO SECRETIONS
It is not enough simply to look at a patient’s eyelids. Many patients whose lid margins appear to be normal have obstructed or inspissated glands, so diagnostic expression is important. If a clinician tries to express the glands and obtains no secretions or thick, toothpaste-like secretions, the patient likely has MGD (Video 1).
Video 1. A patient undergoes diagnostic expression of the meibomian glands. The thick, toothpaste-like secretions are an indication of meibomian gland dysfunction. Video credit: Alice Epitropoulos, MD.
In some cases of MGD, little meibum will be expressed initially, but continued pressure may suddenly unblock one or more glands (Video 2). The quality of the meibum may subsequently improve so that the glands begin expressing the clear lipids that are necessary for tear film stability and homeostasis.
Video 2. In some patients, continued pressure may be required to clear an obstructed meibomian gland (area in circle). Video credit: Marjan Farid, MD.
Ensuring that the meibomian glands are unobstructed is one of the first steps in treating MGD; manual expression and VTP therapy are two good options to accomplish this goal. Maintenance therapy—including Bruder microwavable masks (Bruder), warm compresses, microblepharoexfoliation, lid scrubs, and omega-3 fatty acid supplementation—will work better if the glands are unobstructed.
EARLY MEIBOMIAN GLAND DYSFUNCTION
A 36-year-old woman who wears contact lenses presented with a complaint of bilateral stinging, foreign body sensation, tearing, and eye fatigue and burning in the evening. The patient stated that the symptoms were present whether or not she was wearing her contact lenses, and she expressed a desire to wear contact lenses for more time than her discomfort allowed. She had a SPEED score of 20. Tear breakup time was 4 seconds in both eyes, suggesting an unstable tear film consistent with evaporative DED secondary to MGD.
Given that this patient was not using prescribed DED therapy or artificial tears, a conservative approach was warranted. She began using lipid-containing artificial tears, 2 g daily reesterified omega-3 nutritional supplements, and a Bruder microwavable mask for 5 minutes twice per day. The patient’s symptoms improved in 6 weeks, and she felt more comfortable in her contact lenses. This regimen is a good first step for someone who hasn’t yet tried other treatments or who may not have access to other technologies.
DON’T BE AFRAID TO REFER A PATIENT
Some providers, particularly younger ones, may not have access to all of the technology discussed in this article, such as VTP or microblepharoexfoliation. In the event that one of these clinicians encounters suspected DED secondary to MGD, a referral to a dry eye specialist is suggested. The authors urge clinicians who do have access to the technologies mentioned in this article to use such innovations.
- Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31:472-478.
- Trattler WB, Majmudar PA, Donnenfeld ED, et al. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.
- Cochener B, Cassan A, Omiel L. Prevalence of meibomian gland dysfunction at the time of cataract surgery. J Cataract Refract Surg. 2018;44:144-148.
- Gupta PK, Stevens MN, Kashyap N, Priestley Y. Prevalence of meibomian gland atrophy in a pediatric population. Cornea. 2018;37(4):426-430.
- Epitropoulos AT, Matossian C, Berdy GJ, et al. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015;41:1672-1677.