Cataract surgery is the most commonly performed surgical procedure in the United States. Millions of cataract surgeries have been performed—and the annual number surgeries will rise each year as life expectancy increases. Advances and new technologies are constantly being explored to further improve patient outcomes and quality of life.
With these advances in technology, modern cataract surgery has adopted a secondary focus: refractive cataract surgery. Although the main objective of the procedure is to remove the opacified natural lens, we now have the means to help patients become more spectacle independent postoperatively. New lens designs, such as toric and multifocal modalities, have revolutionized cataract surgery.
To determine whether a given patient is a good candidate for such options requires not only routine cataract diagnostic tests, but also attention to other examinations and to details of the patient’s personality.
When the cataract evaluation is complete, the next step is to have an educational discussion with the patient regarding his or her surgery and lens options. After this educational discussion, I address any ocular surface issues. These can have a significant impact on lens selection, refractive outcomes, and patient satisfaction postoperatively.1
I also take time to learn more about the patient—hobbies, lifestyle, personality traits, etc. It is our responsibility to present all the surgical options to every patient, as we don’t truly know their goals or financial situation. One should understand the patient’s desires and expectations regarding wearing or avoiding glasses after surgery. Setting appropriate postoperative expectations is key to patient satisfaction.
IOL OPTIONS
In my discussion of IOL options with the patient, I first discuss standard monofocal IOLs. I never try to down-sell this option, as outcomes with even standard lenses nowadays are outstanding. However, I counsel that the patient may need glasses after surgery to achieve the sharpest vision at distance and will definitely need them for near vision.
I next discuss the topic of astigmatism. If the patient has more than approximately 0.75 D, then I discuss how correcting this at surgery can help eliminate the need for distance glasses. Correction can be achieved via limbal relaxing incisions (also known as LRIs) or, if the power of their astigmatism is greater than approximately 1.25 D, a toric IOL. Of course this choice is surgeon-dependent and influenced by the location and size of the main incision, as some flattening of the cornea in this meridian can be induced by the surgery itself.
One alternative to standard monofocal cataract surgery, I tell the patient, is blended vision or monovision, which is still achieved with monofocal IOLs. Monovision is great for most individuals who have used this strategy in the past with contact lenses or refractive surgery. What I term semi-monovision (typically a target of -0.75 D to -1.25 D in the nondominant eye) provides the added benefit of spectacle-free intermediate vision as well as improved depth perception compared with full monovision. However, patients who choose this option will still need reading glasses for fine print and for longer periods of reading. In my experience, patients adapt to semi-monovision much more easily than to true monovision.
This brings me to the final lens option I discuss: multifocal IOLs. Older multifocal and accommodating IOLs, such as the Crystalens (Bausch + Lomb), the »AcrySof Restor (Alcon), and »Tecnis Multifocal (Johnson & Johnson Vision) provided good vision at distance, intermediate, and (sometimes) near. However, they had major issues that complicated the comanagement process, including glare and halos when driving at night, uncorrected astigmatism, and the need to adapt to a completely new set of optics. Older technology multifocal IOLs achieved different zones of focus by splitting up light that enters the eye, which led to decreased contract sensitivity. This decrease in contrast sensitivity is often subjectively conveyed by patients as less crisp vision. Therefore, when presenting these older multifocal lenses to patients, I would always include a caveat: They involve a compromise in vision, with less spectacle dependence in return for a slight decrease in the quality of vision.
A RECENT ENTRY
A recent entry to this market is the »Tecnis Symfony IOL (Johnson & Johnson Vision), which is categorized by the manufacturer as an extended depth of focus implant. Its technology, which is said to provide a broader range of vision and improved quality of vision, corrects chromatic and spherical aberrations in the eye (Figure). The lens is also available in a toric version that can correct most levels of astigmatism. The Symfony lens has an elongated range of focus, reducing the halos and glare that brought many patients back into our offices with complaints with older lens models. It also uses achromatic technology that corrects chromatic aberration, providing sharper overall vision.
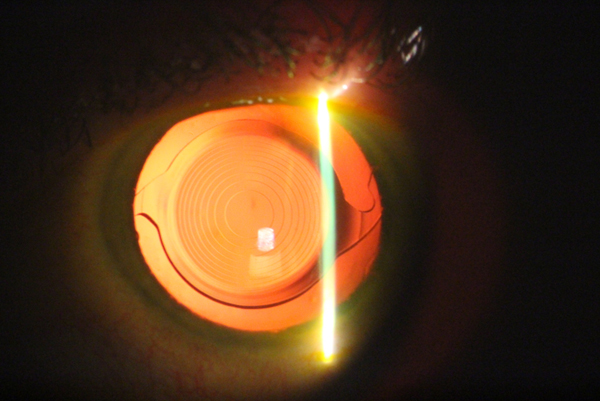
Figure. The Symfony IOL in situ after implantation.
As promising as this new technology is, it is still important to discuss expectations with patients about this lens. Distance vision with the Symfony IOL is unremarkable. In my experience, 20/20 distance vision is the norm with patients postoperatively. Intermediate vision ranges from 20/16 to 20/32 in most of the patients I have comanaged. Near vision is typically 20/32 to 20/50.
One may find those statistics for near vision less robust than might be desired for a multifocal IOL. However, remember that this lens provides an extended depth of focus and is not designed to provide perfect uncorrected near vision. The patient will need a small reading prescription. If this point is conveyed to patients before surgery, then they are completely thrilled with their outcomes. However, if they are sold on having a multifocal lens that will provide complete spectacle independence, then they will be less than satisfied. Some patients achieve complete spectacle independence, but I consider this a bonus to an already superb outcome.
Ultimately, there are two matters of discussion to set up success with the Symfony lens. First, patient selection is crucial. Second, education and setting expectations for the lens (to the point of almost underselling it) will facilitate a smooth comanagement process and allow patients to truly love and appreciate their new vision.
- Afsharkhamseh N, Movahedan A, Motahari H, et al. Cataract surgery in patients with ocular surface disease: an update in clinical diagnosis and treatment. Saudi J Ophthalmol. 2014;28(3):164-167.






