
Diabetic retinopathy (DR) is the leading cause of blindness in the United States in patients 20 to 74 years old.1 It affects 28.5% of the US population 40 years and older.2 Optometrists encounter many patients with diabetes. It is important to be aware of the risks that lead to DR and to be ready to offer recommendations to our patients.
PATHOPHYSIOLOGY OF DR
The pathophysiology of DR is not well understood and is believed to be multifactorial. The primary cause of damage in DR is thought to be long-term hyperglycemia, which leads to vascular endothelial cell damage, inducing vascular permeability and vascular occlusion. Vascular permeability leads to macular edema. Vascular occlusion leads to ischemia, which, in turn, may cause retinal tissue to trigger the release of vascular endothelial growth factor (VEGF), leading to neovascularization.3
STAGES OF DR AND RECOMMENDED FOLLOW-UP
DR is categorized as nonproliferative DR (NPDR) and proliferative DR (PDR); the absence of neovascularization indicates the former, and its presence indicates the latter. Further differentiation for NPDR, based on its severity, is important for proper follow-up and management (see sidebar on the next page for details).
The recommended follow-up for patients with NPDR is based on risk of progression. Risk of progression to PDR at 1 year is 5% for patients with mild NPDR, 15% for moderate NPDR, and 52% for severe NPDR.1 Therefore, the recommended follow-up is 1 year for mild NPDR and 6 months for moderate NPDR. Due to the 50% risk of severe NPDR leading to PDR within 1 year, these patients should be considered for referral to a retina specialist.
PDR is ultimately determined by the presence of neovascularization, which may manifest on the optic disc (neovascularization of the disc) or elsewhere in the retina (neovascularization elsewhere). Neovascularization may lead to preretinal hemorrhage, vitreous hemorrhage, and tractional retinal detachment. PDR is categorized as non–high risk and high risk. The Diabetic Retinopathy Study found that early treatment of non–high risk PDR with panretinal photocoagulation reduced risk of severe vision loss by 50%, which underscores the need for early intervention by a specialist.4
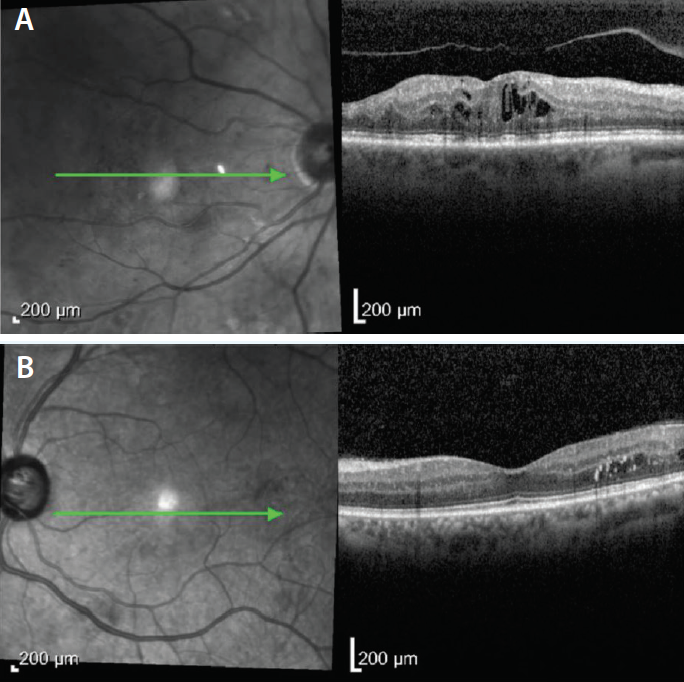
Figure. OCT scan of a diabetic patient with center-involving macular edema (A). OCT scan of a diabetic patient with noncentral macular edema (B). Note the presence of intramacular exudates.
MACULAR EDEMA
Macular edema can develop at any stage of DR. For optometrists without access to optical coherence tomography (OCT), familiarity with the Early Treatment of Diabetic Retinopathy Study (ETDRS) definition of clinically significant macular edema (CSME) is important; this finding should lead to referral to a retinal specialist for treatment. Macular edema that is not clinically significant should be monitored every 3 to 4 months. CSME is defined as one of the following:
- retinal edema located at or within 500 µm (1/3 disc diameter, or DD) of the center of the macula;
- hard exudates at or within 500 µm of the center of the macula, if associated with thickening of the adjacent retina; or
- a zone of thickening larger than 1 disc area located within 1 DD of the center of the macula.
As more optometrists obtain access to OCT imaging, it becomes less important to define CSME and more important to focus on whether or not macular edema is center-involving (Figure). Center-involving macular edema leads to decreased vision and requires treatment. If center-involving macular edema is mild and does not affect a patient’s vision, treatment is not indicated. In these situations, patients should be monitored with OCT every 2 to 4 months. Noncentral macular edema should be referred for treatment if disease is severe and continually increasing, regardless of the effect on the patient’s vision.
RISK FACTORS FOR PROGRESSION OF DR
Two risk factors associated with incidence and progression of retinopathy are duration of diabetes and poor glycemic control. Researchers in the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) reported a 10-year incidence of DR in more than 70% of patients with type 1 or type 2 diabetes.5 Patients with type 1 diabetes were more likely to have DR findings and were more likely to progress to PDR compared with patients with type 2 diabetes.5
Recent clinical trials suggest that the incidence and progression of PDR in diabetic patients has decreased two- to threefold over the past several decades. No large population studies have been conducted recently, but researchers in the WESDR found that patients enrolled in the 1990s showed reduced incidence and progression compared with those enrolled in the 1980s. This finding is likely due to better control of risk factors, earlier detection, and availability of more effective ocular therapies.6
If hypertension is poorly controlled for years, the risk of progression of DR and diabetic macular edema is increased. Carotid artery disease can also exacerbate PDR due to ischemia of ocular tissue.
Hormonal changes in the body during pregnancy may trigger DR or cause progression of existing DR. Women with PDR at the time of conception should be referred for treatment. Women with NPDR at the time of conception rarely progress to PDR, but they should be monitored closely nevertheless, as development of PDR should prompt referral. Macular edema can also be triggered during pregnancy, although it tends to regress spontaneously thereafter and typically requires only monitoring.7
WHY WE NEED TO KNOW ABOUT DR
Understanding the levels of severity of DR allows optometrists to conduct appropriate follow-up, management, and referral. It is important to realize that severe vision loss is often preventable with proper treatment. Patients must understand the importance of keeping appointments as recommended and should be encouraged in their journey with diabetes.
- Fraser CE, D’Amico DJ. Diabetic retinopathy: Classification and clinical features. UpToDate. Wolters Kluwer. Retrieved May 26, 2017. www.uptodate.com/contents/diabetic-retinopathy-classification-and-clinical-features.
- Zhang X, Saaddine JB, Chou C, et al. Prevalence of diabetic retinopathy in the United States, 2005-2008. JAMA. 2010;304(6):649-656.
- McCulloch DK. Diabetic retinopathy: Pathogenesis. Wolters Kluwer. Retrieved May 26, 2017, www.uptodate.com/contents/diabetic-retinopathy-pathogenesis.
- Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology. 1981:88(7):583-600.
- Klein R, Klein BEK, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of diabetic retinopathy. XIV. Ten-year incidence and progression of diabetic retinopathy. Arch Ophthalmol. 1994;112(9):1217-1228.
- Liew G, Wong VW, Ho IV. Mini review: Changes in the incidence of and progression to proliferative and sight-threatening diabetic retinopathy over the last 30 years. Ophthalmic Epidemiol. 2017;24(2):73-80.
- Pescosolido N, Campagna O, Barbato A. Diabetic retinopathy and pregnancy. Int Ophthalmol. 2017;34(4):989-997.

