
Cataract surgery is now refractive surgery. We have heard this for years. But do eye doctors really get it? Are we doing a good enough job of properly screening our patients for ocular surface disease (OSD) prior to surgery? We need to rethink practice habits that we have been using for decades.
Should we delay surgery for patients with OSD, or should we continue, as we have done, to schedule them for surgery in the next available time slot, usually just a few weeks after an initial consultation? This is an emerging dilemma, now that new technologies have given us a better chance of achieving the best surgical outcomes for our patients, as long as other variables such as OSD are treated first.
Advances in technology have contributed to the evolution of refractive cataract surgery, allowing it to become one of the most commonly performed surgeries in the United States. These advances have allowed this once-routine surgical procedure to live up to its promise as a refractive procedure. Technologies such as premium IOLs, femtosecond lasers, 3-D and wavefront intraoperative diagnostics, and highly accurate biometry diagnostics give surgeons the tools necessary to deliver the best possible outcomes
NO MORE GLASSES
Just a few decades ago, a common and accepted surgical outcome would leave patients with residual refractive errors of 1.00 D to 2.00 D. These patients were happy wearing glasses after surgery because this was the norm. Patients had low expectations for surgeons, especially regarding accurate calculation of IOL powers to reduce residual refractive error.
Those days are over. Patient expectations are higher than ever, even for nonpremium monofocal IOLs. Patients who elect presbyopia-correcting options, such as multifocal, accommodating, and extended depth of focus IOLs, expect to have good vision at all ranges of distance, with little to no dependence on glasses.
With increased use of advanced technologies among surgeons, why do we sometimes end up with unhappy patients after refractive cataract surgery? I believe residual refractive error is the leading cause. Sometimes surgeons miss the target, leaving residual refractive error, which contributes to blur, limits vision, increases symptoms of glare and halos, and reduces contrast sensitivity.
I also believe that a leading cause for incorrect IOL calculation is untreated OSD, which limits the accuracy of biometry. OSD can limit the accuracy of preoperative tests such as corneal topography and biometry,1and bad inputs into IOL calculation formulas lead to bad outputs. Untreated preoperative OSD may lead to residual refractive error; some patients will perceive decreased vision with errors as small as 0.50 D. Significant uncontrolled OSD can lead to higher residual refractive errors, as much as 1.00 D to 2.00 D, due to its effect on preoperative calculations.
HIGH PREVALENCE
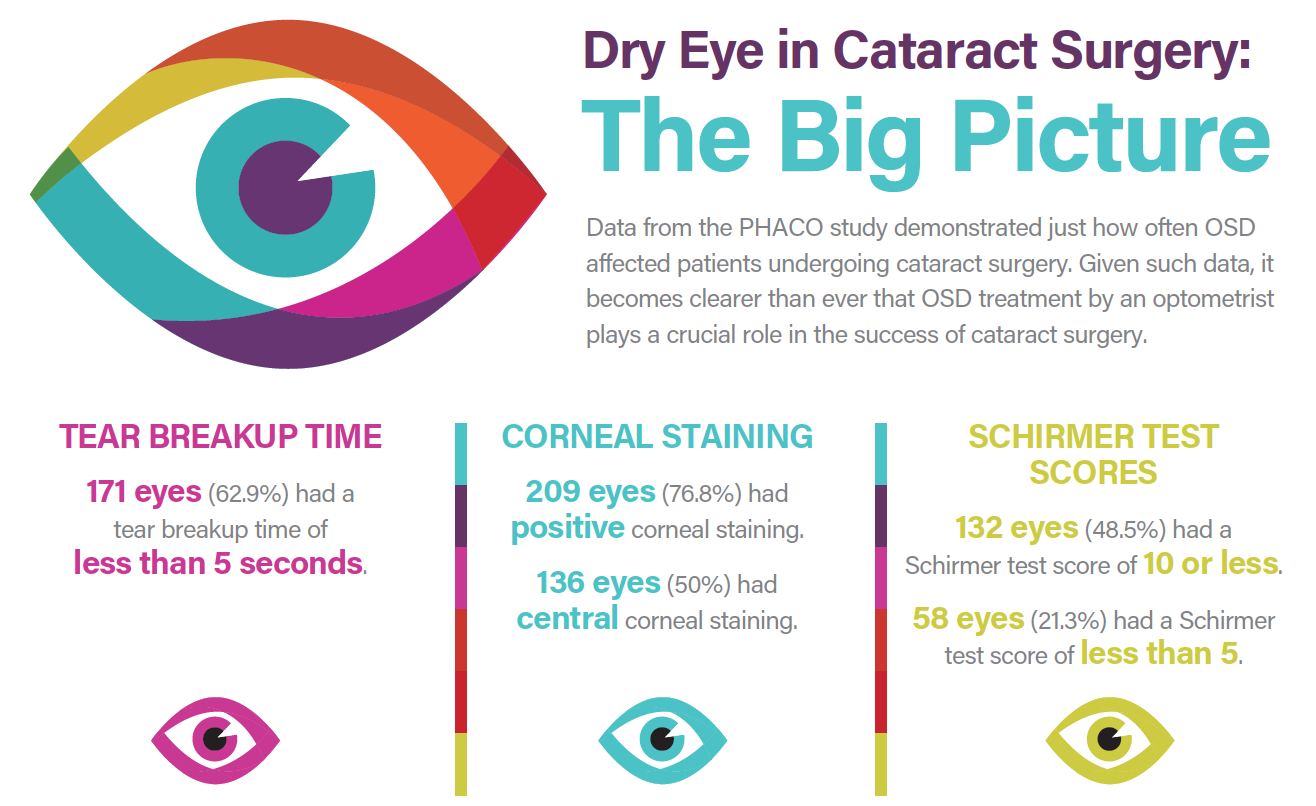
The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study showed just how commonly cataract patients are affected by OSD.2 The purpose of the study, which included 136 patients (272 eyes), was to determine the prevalence of dry eye disease in patients undergoing cataract surgery. The results showed that about two-thirds of eyes had tear breakup time of less than 5 seconds, half of eyes showed central corneal staining, three-quarters of eyes had positive corneal staining, and nearly half of eyes had a Schirmer test score of 10 or less. (To explore data from the PHACO study in more detail, see the infographic Dry Eye in Cataract Surgery: The Big Picture below.)
Not only do cataract patients have a higher percentage of clinically significant eye dryness and meibomian gland dysfunction, but also these two chronic diseases are often ignored and not properly diagnosed and treated before surgery. Blepharitis is also common in cataract patients. A study by Luchs et al looked specifically at the prevalence of blepharitis in patients having cataract surgery and found that 59% of patients were affected by this condition.3
Increased age is one of the largest risk factors for dry eye, just as it is a risk factor for cataract. With a high prevalence of OSD among cataract patients, we must actively examine, diagnose, and treat these patients before performing biometry. This is not a new recommendation, and it is considered the standard of care; however, it is rare to see patients have their surgeries delayed so that their OSD can be better managed.
PARADIGM SHIFT
Cataract surgery has evolved into a refractive surgical procedure, giving patients more options than ever. Modern treatment options are safe and accurate and can treat all types of refractive errors. A paradigm shift must occur so that surgeries are being delayed to treat OSD first, not scheduled as soon as possible as is commonly done.
We must actively examine cataract surgery candidates for OSD and begin treatment before biometry and surgery. This practice will lead to more accurate IOL power calculations with better outcomes and less residual refractive error.
- Kaufman HE. The practical detection of MMP-9 diagnoses ocular surface disease and may help prevent its complications. Cornea. 2013;32(2):211-216.
- Trattler W, Reilly C, Goldberg D, et al. Cataract and dry eye: prospective health assessment of cataract patients’ ocular surface study. Poster presented at: American Society of Cataract and Refractive Surgery Annual Meeting; March 25-29, 2011; San Diego.
- Luchs J, Buznego C, Trattler W. Prevalence of blepharitis in patients scheduled for routine cataract surgery. Poster presented at: ASCRS Symposium on Cataract, IOL, and Refractive Surgery; April 11, 2010; Boston, MA.

