
Well, that didn’t turn out as planned. Now what?
It happens to even the best surgeon after the most well-calculated and perfectly performed surgery: postoperative toric IOL surprise. The most common sources of toric refractive surprise include preoperative miscalculation of refractive magnitude, pseudoastigmatism, miscalculation of effective lens position in eyes with axial lengths less than 22.5 mm, malposition of the toric IOL, and noncorneal sources of astigmatism.
When the residual refractive error indicates that there is cylinder or that cylinder is outside expectations, it is important to investigate the cause. Start with a thorough examination of the corneal surface and repeat topography and biometry. Follow with dilated examination and optical coherence tomography imaging to examine the lens positioning and the macula.
Once the cause is identified, options can be explored, and a great surgical outcome and patient satisfaction can still be achieved.
OPTIMIZE THE CORNEAL SURFACE
Pseudoastigmatism may be caused by any ocular surface irregularity, including dry eye disease, pterygium, epithelial basement membrane dystrophy (EBMD), and Salzmann nodular degeneration. It is important to identify and aggressively treat these conditions in order to mitigate any possible resulting changes in refractive error that may be reversible (Figure 1).
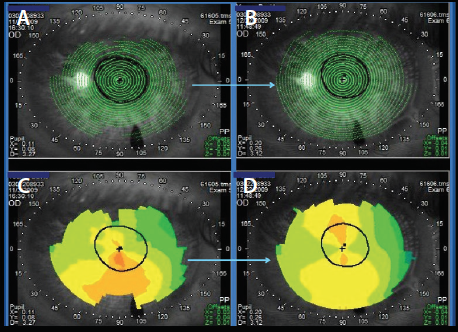
Figure 1. This patient’s initial topography (C) shows possible inferior cornea steepening. Note that the Placido disc rings for this image (A) were of poor quality and incomplete toward the periphery. In the same patient after treatment for dry eye, the Placido rings demonstrate better quality (B) and the topography does not have the inferior steepening seen in the previous test (D).
Postoperative drops are known to cause ocular surface dryness, more so in patients who had preexisting ocular surface disease.1-3 For treatment of this dryness, the clinician can consider punctal occlusion, preservative-free topical steroids, lifitegrast ophthalmic solution 5% (Xiidra, Shire), cyclosporine ophthalmic emulsion 0.05% (Restasis, Allergan), a low-dose topical steroid such as loteprednol etabonate ophthalmic suspension 0.5% (Lotemax, Bausch + Lomb), oral omega-3 fatty acid supplementation, and lid scrubs and warm compresses as appropriate.4 The use of amniotic membrane can also be considered in these cases to maximize corneal health.
If the patient has a pterygium, consider having it removed before deciding on any enhancements, knowing that this is a progressive issue that may change the patient’s refractive error in the future.5-7In corneal surface abnormalities such as EBMD or Salzmann nodular degeneration, aggressive lubrication or other ocular medications may not improve the surface, in which case performing a lamellar keratectomy should be considered. Remember to look for subtle EBMD, which is easier to pick up on slit-lamp examination by looking for negative staining with the cobalt blue filter (Figure 2).
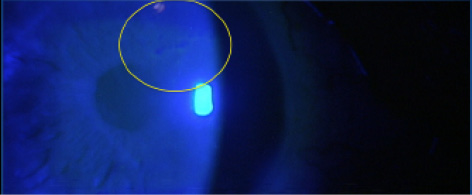
Figure 2. Note the subtle epithelial basement membrane dystrophy in this patient, shown by the negative fluorescein staining pattern.
IF THAT STILL DIDN’T FIX IT
Once we have eliminated any sources of pseudoastigmatism, confirmed that there is no macular disease, and made sure the IOL is not tilted, it is time to consider surgical options for correcting the patient’s refractive surprise.
For patients who have less than 1.25 D of residual astigmatism, a corneal or limbal relaxing incision (LRI) or IOL realignment can be considered for those who have a misaligned premium toric IOL.8 For patients who have more than 1.50 D residual astigmatism, realignment, IOL exchange, or laser vision correction may be considered.8 An online Toric Results Analyzer (www.astigmatismfix.com) developed by John Berdahl, MD, and David R. Hardten, MD, can help to determine whether rotation of a misaligned lens would improve the patient’s residual refraction and, if so, how much to rotate the lens.
As an example: A patient presented at his 1 month postoperative visit after cataract extraction with implantation of a toric posterior chamber IOL. His uncorrected distance visual acuity (UDVA) in the operated eye was 20/60+. The patient had a residual manifest refraction of -0.75 +1.50 X 150. He had been implanted with a 19.00 D T4 AcrySof IQ Toric IOL (Alcon) at 175°. Upon dilated examination, the toric IOL was noted to be aligned at 033°. After evaluating the patient (Figure 3) and using the aforementioned Toric Results Analyzer (Figure 4), it was decided that rotating the patient’s lens was the optimal approach to addressing the misalignment. At 1 week after rotation of the IOL, the patient’s UDVA was 20/20 in the operated eye with a refraction of -0.25 D sphere.
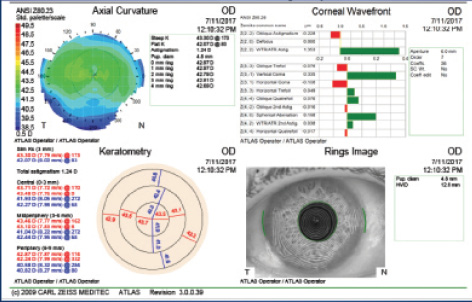
Figure 3. Postoperative topography (Atlas 9000; Carl Zeiss Meditec) demonstrates 1.24 D of anterior corneal astigmatism at 173°.
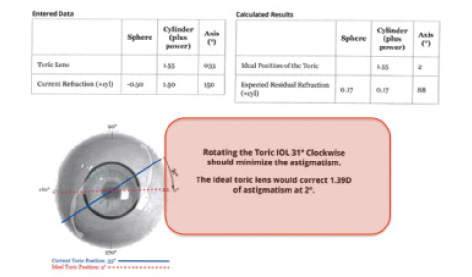
Figure 4. Calculations for this patient from the website www.astigmatismfix.com website, using the formulas developed by Berdahl and Hardten. The program suggests that the patient should have his lens rotated 31° clockwise to minimize the residual astigmatism.
Corneal relaxing incisions or LRIs can be used to correct residual mixed astigmatism, which may exist as either an undercorrection or an overcorrection of the patient’s original refractive error. The choice of whether to create new LRIs, as opposed to opening existing LRIs, depends solely on the current refractive error. If the patient’s axis of cylinder has flipped, LRIs may actually compromise the patient’s quality of vision.
If laser vision correction is warranted, it is important to wait at least 2 to 3 months after the cataract surgery to allow wounds to heal and LRIs to settle. Before laser vision correction is performed, it is a good idea to perform Nd:YAG posterior capsulotomy.
GIVE UP AND TRY AGAIN?
When is it time to exchange the patient’s IOL? This should be considered if the patient is experiencing poor quality of vision, negative dysphotopsia, or other IOL-related issues. Exchange may be warranted if the patient’s residual astigmatism or spherical equivalent is off by more than 1.25 D. Exchange should also be considered in patients who are not good candidates for LRIs or laser vision correction.
Make sure to take all appropriate steps to decrease any possible causes of pseudoastigmatism before revision surgery. Taking the time to address corneal irregularities and ocular surface disease can avoid added patient frustration and postoperative chair time. When there are other causes of residual astigmatism in the toric IOL patient, assess the patient’s best options for correction, and, in the end, patient satisfaction and optimal vision are still obtainable.
- Ali MA, Abdelhalim AS. Ocular surface changes after simultaneous cataract surgery and limbal relaxing incisions. Journal of the Egyptian Ophthalmological Society. 2017;110(1):28-30.
- González-Mesa A, Moreno-Arrones JP, Ferrari D, Teus MA. Role of tear osmolarity in dry eye symptoms after cataract surgery. Am J Ophthalmol. 2016;170:128-132.
- Sutu C, Fukuoka H, Afshari NA. Mechanisms and management of dry eye in cataract surgery patients. Curr Opin Ophthalmol. 2016;27(1):24-30.
- Mohammadpour M, Mehrabi S, Hassanpoor N, Mirshahi R. Effects of adjuvant omega-3 fatty acid supplementation on dry eye syndrome following cataract surgery: a randomized clinical trial. J Curr Ophthalmol. 2016;29(1):33-38.
- Sheppard JD, Mansur A, Comstock TL, Hovanesian JA. An update on the surgical management of pterygium and the role of loteprednol etabonate ointment. Clin Ophthalmol. 2014;8:1105-1118.
- Hirst L. Distribution, risk factors, and epidemiology. In: Taylor HR, ed. Pterygium, Vol. 2. The Hague: Kugler Publications; 2000: 15-28.
- Lin A, Stern G. Correlation between pterygium size and induced corneal astigmatism. Cornea. 1998;17(1):28-30.
- Nanavaty MA, Bedi KK, Ali S, et al. Toric intraocular lenses versus peripheral corneal relaxing incisions for astigmatism between 0.75 and 2.5 diopters during cataract surgery. Am J Ophthalmol. 2017;180:165-177.

