

Objective diagnostic instruments are playing an increasingly important role in glaucoma management. These tools allow optometrists and ophthalmologists to detect and treat glaucoma at earlier stages of the disease than was possible with older diagnostic modalities and to identify specific pathology for targeted treatment.
Historically, glaucoma diagnosis relied heavily on intraocular pressure (IOP) readings; however, glaucoma is multifactorial, and there can be significant variability from patient to patient in the level of IOP that is truly indicative of disease. Employing multiple objective diagnostic tools to monitor trends and fluctuations in nerve function and structure can help us make sense of subjective and objective data to determine the urgency of treatment and the best modality for that treatment.
A MULTIFACETED APPROACH
Detection and diagnosis of glaucoma requires more than just an IOP check. Identifying patterns and trends in visual function and reconciling these against the condition of the nerve structure can help to identify the disease in its early stages. In our collaborative optometry-ophthalmology practice model, we use a mix of diagnostic technologies to provide objective data that can be shared by our practitioners.
We perform progression analysis using optical coherence tomography (OCT) on the Spectralis (Heidelberg Engineering). The Spectralis performs full posterior mapping and analysis of the macula and allows the user to compare images taken over time to a patient’s baseline image. The visual and quantitative data facilitate the detection of changes within the retinal nerve fiber layer around the macula, which may be indicative of pattern changes around the retinal nerve (Figure).
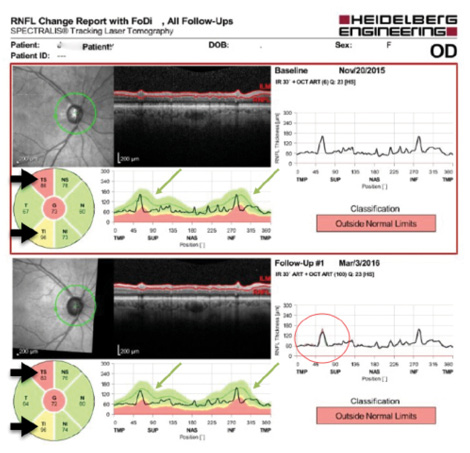
Figure. Example of a right eye retinal nerve fiber layer (RNFL) progression analysis with OCT, which helps doctors objectively assess stability versus progression in glaucoma. The thick black arrows indicate quantitative analysis of thinning RNFL sectors; the data similarity at baseline and in follow-up indicate stability. The thin green arrows indicate corresponding thinning as shown on an RNFL plot. The area in the red circle indicates that there has been a minimal change in the superotemporal sector. This is an area to watch for disease progression, which can be done on the next OCT scan, in correspondence with visual field testing changes in the inferonasal area, and in the clinic via nerve assessment.
We use the Diopsys Nova (Diopsys) to perform pattern electroretinography (pERG). Use of pERG allows us to identify stressed retinal ganglion cells at the subclinical stage, when the cells have become dysfunctional but are still alive. When we see reduced retinal function on pERG, we can begin aggressive treatment aimed at slowing disease progression. After treatment is initiated, pERG allows us to measure functional loss or recovery and adjust treatment accordingly.
Patients who are glaucoma suspects or who have borderline or conflicting results on other diagnostic tests may benefit from visual electrophysiology testing. pERG aids us in the “to treat or not to treat” decision-making process, when we encounter visual field findings that do not seem to correlate with the nerve structure. Abnormal pERG results can identify pathology, such as low-tension glaucoma, that might otherwise go undetected due to normal IOP readings. pERG testing can also assist in determining whether disease is in the retina or in the visual pathway when used along with visual evoked potential (VEP), which is also performed with the Diopsys Nova. After we determine disease location, we can proceed with appropriate therapy.
MIXED TECHNOLOGY TREATMENT APPROACH
Glaucoma is a complex disease, and one treatment does not fit all patients. Today we have a variety of treatment options, each with a unique mechanism of action. Minimally invasive but highly effective approaches—performed alone, sequentially, or in combination—can have greater efficacy when they are employed before functional capacity is destroyed by diseased structure.
Traditionally, the first line of treatment for glaucoma has been topical ocular hypotensive medications. We know, however, that patient compliance with medication regimens is poor. As an alternative to drops, patients in the early stages of the disease may benefit from nonthermal trabeculoplasty, which goes by different names depending on the laser manufacturer: selective laser trabeculoplasty (SLT; Ellex) and micropulse laser trabeculoplasty (MLT; Iridex). These nondestructive laser procedures leave the possibility for additional repeat treatments or other treatment options as the disease progresses.
When the disease is detected early, minimally invasive glaucoma surgery (MIGS) procedures can be highly effective and extremely safe treatment options. These procedures are often performed in combination with cataract surgery. In our practice, we perform several of these procedures, including use of the Trabectome (NeoMedix), the iStent (Glaukos), the Kahook Dual Blade (New World Medical), the CyPass Micro-Stent (Alcon), and, soon, the Xen Gel Stent (Allergan).
COLLABORATIVE CARE
Providing the highest level of patient care often involves collaboration between ophthalmologists and optometrists, as in our practice. The state-of-the-art diagnostics described above help us to collaboratively manage our patients by providing objective, quantifiable data on each patient. They also reduce the confusion that can result from reliance on subjective information. Depending on the patient’s test results and the comfort level of the practitioner, treatment can proceed under the care of the optometrist, or the patient can be referred to a specialist with a treatment plan such as SLT or MLT already in place.
Successful collaborative patient management requires effective communication and a sense of comfort with one’s collaborator. Our glaucoma team includes two glaucoma specialists and an optometrist whose emphasis is in glaucoma care. We work side by side, with the optometrist included in OR shadowing to observe surgical techniques and clinical shadowing to learn postsurgical management styles. We regularly consult back and forth on cases, and, when concerns arise, we can ensure that patients receive the care they need immediately. By working together and using the optometrist for postoperative management, the surgeons can perform more surgeries. The skill sets of all participants are thus maximized.
Integration of cutting-edge diagnostic technologies improves the standard of care we can offer to our patients. The traditional paradigm of visual field analysis, single time OCT readings, and IOP measurement can produce inconsistent and even contradictory results. Modern technology, such as visual electrophysiology and OCT progression analysis, can provide us with additional objective information to determine the best treatment path. Objective diagnostic data help to ensure that medical collaborators proceed with the same information and to simplify the coordination of care.

