
Refractive surgery represents the best of integrated eye care. Optometrists and ophthalmologists practice to the full scope of their abilities and work cohesively together to enhance their patients’ quality of care. Over all the years, I’ve been involved in refractive surgery, and due in part to better technology and improvements in how we screen and care for patients throughout the process, I have seen outcomes improve dramatically.
MULTIPLE TOUCHPOINTS
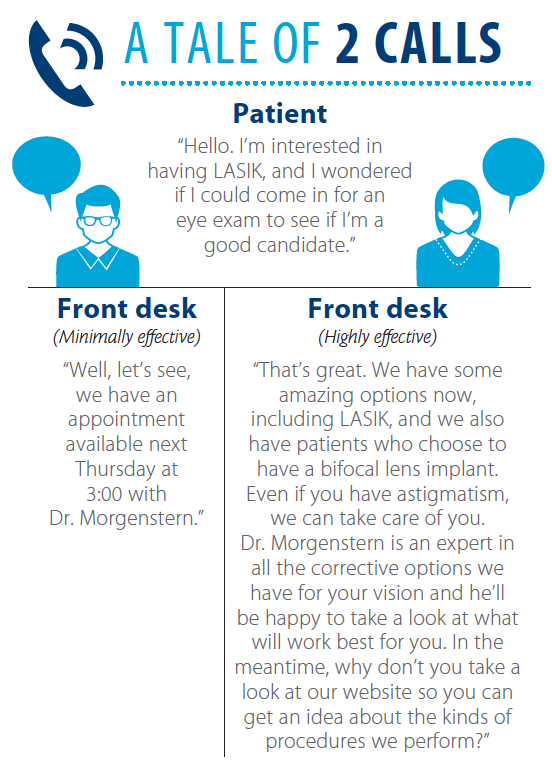
One of the toughest things for many doctors to recognize is that effective patient education doesn’t start with us. The front desk is the most important step in the patient education process because that very first interaction sets the tone for everything that follows.
Often, front desk personnel ask the reason for the call and make an appointment, but that touchpoint can be more effective if the receptionist can direct patients to information, convey enthusiasm, and begin to set expectations about the range of procedures available (Figure). If appropriate, the receptionist should then tag the chart as “Interested in refractive surgery.”
During the appointment, the technician who brings the patient back can continue that enthusiasm and education. He or she can say something like, “I see you are interested in corrective options,” wait for the patient to respond affirmatively, and then say “Oh, our patients love it. Dr. Morgenstern will take great care of you.” Additionally, patient education videos can be shown during any wait time in the office.
With all that, patients are already well-educated by the time I see them. They are excited about the opportunities, aware of the procedures and technology, and already expecting to be talking with me about refractive surgical options—which might be LASIK, but might also be lens surgery.
SETTING EXPECTATIONS
In talking with patients about what they want and expect from refractive surgery, I start out being very general and then, with data and information specific to the patient, I expand upon their goals and expectations.
I want to understand what is bothering the patient and what motivated him or her to come in so that I can tailor my recommendation to him or her. I like to share the outcomes of the PROWL study with patients, which looked at objective and subjective results in hundreds of patients from both military and civilian populations. The percentage of patients with 20/20 vision after surgery was nearly 100% (99% in PROWL-1 and 96% in PROWL-2), and the rate of complications was exceedingly low. Patient-reported outcomes (also termed PRO, which is a fancy way of saying “opinions”) were also very positive, with more than 96% of patients reporting satisfaction at 3 months.1
It is particularly important to discuss presbyopia, which, in my experience, is the biggest contributing factors to dissatisfaction with LASIK. If the patient’s expectations of good uncorrected vision at all distances weren’t realistic, it could be that we failed to do a satisfactory job helping him or her to understand that there will still be a need for reading glasses now or in the future.
THE VALUE OF CREATIVE LANGUAGE
Medical terminology is difficult for most patients to absorb. It doesn’t mean they are stupid or not paying attention—it is just a language they don’t speak. The onus is on us to translate what we know into something the layperson can understand. My approach is to use analogies to help patients relate what I’m saying to something they understand better. These make more sense to the patient than a clinical discussion using phrases such as reducing pathogen load on the ocular surface and tear film homeostasis.
For example, when I talk about the importance of treating ocular surface disease (OSD), I ask, “If you were going to have abdominal surgery, would you want the surgeon to cut into red, irritated, flaky skin that doesn’t heal well or into healthy skin?” Or sometimes I will tell them that doing surgery without taking care of their OSD is like a boxer going into a fight without training.
In my practice, OSD treatment always starts with good lid scrubs and, many times, hypochlorous acid to decrease normal bacterial load. A preoperative regimen might include artificial tears, topical therapies, or other treatments.
TECHNOLOGY CHOICES
Patients rarely choose a doctor or surgery center based on a specific technology. In my experience, they choose based on reputation, but that still ties back to technology. Over the years, I’ve found that the iLASIK technology suite (Johnson & Johnson Vision) provides an excellent opportunity to achieve the kind of outcomes that drive word-of-mouth referrals and build our reputation. Since the early days of the Star S2 laser, this platform has continually grown more sophisticated.
Even the best racecar driver needs a great car to win the race. If you put Mario Andretti in a Volkswagon Beetle, his professional skills are not optimized and he is not going to win the race. Similarly, refractive surgery demands both the right surgeon and the right technology.
Good patient screening and treatment of OSD help ensure that we have qualified candidates who will be able to achieve good outcomes from laser or lens-based refractive surgery. Referring to surgeons whose reputation has been built on great technology is key, and educating patients effectively—in language they can understand—is essential to maintaining realistic expectations and high levels of satisfaction after surgery.
- Eydelman M, Hilmantel G, Tarver ME, et al. Symptoms and satisfaction of patients in the patient-reported outcomes with laser in situ keratomileusis (PROWL) studies. JAMA Ophthalmol. 2017:135(1);13-22.

