
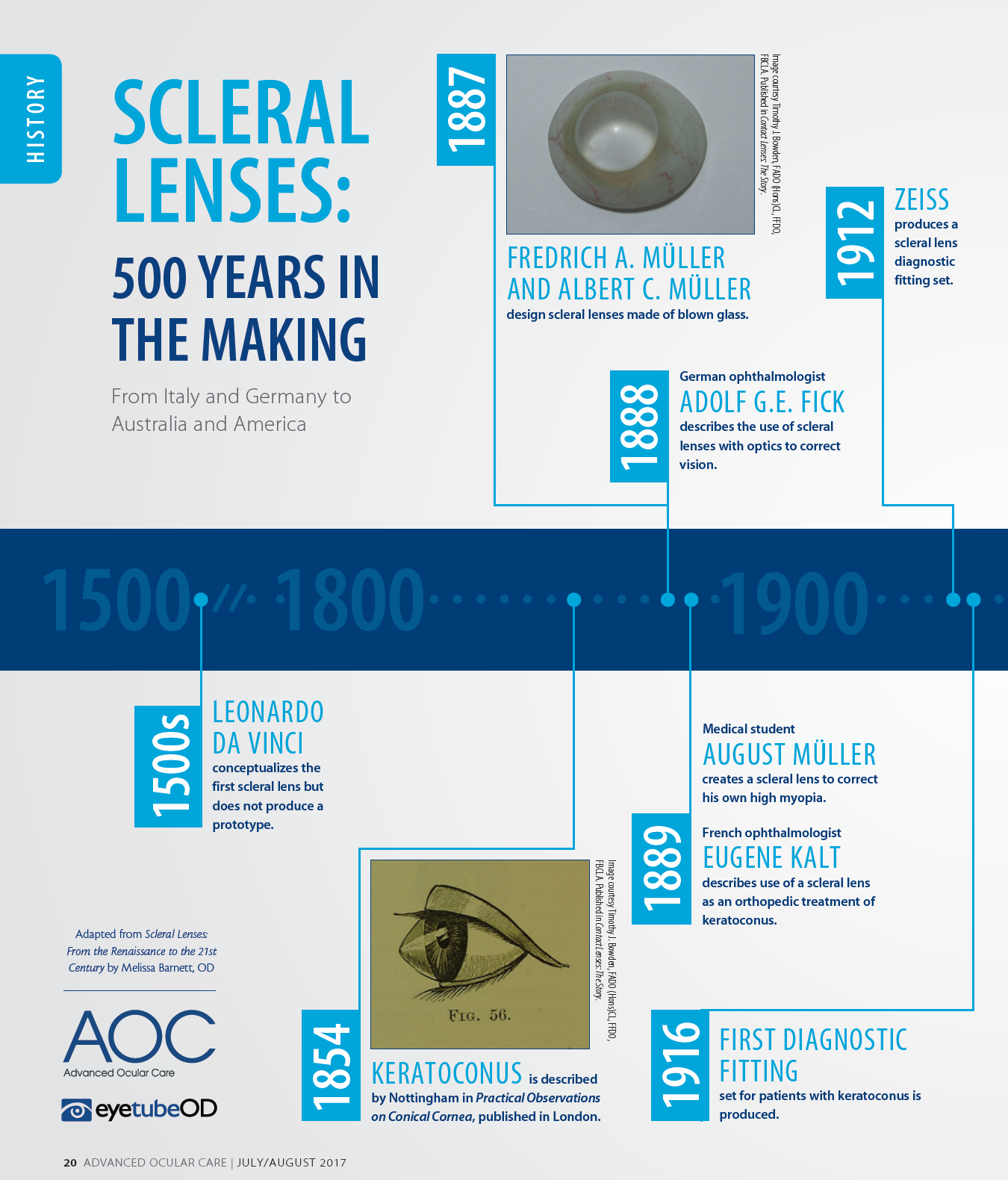
Scleral lenses have experienced tremendous growth in recent years. The earliest type of contact lenses manufactured, scleral lenses are designed to vault the entire corneal surface and rest on the conjunctival and scleral tissue. Before innovators push the boundaries of scleral lenses even further, we should all indulge our curiosity in the history of scleral lenses that have helped countless patients over the past half millennium—and could help hundreds of thousands more in the future.
GOOD IN CONCEPT, LACKING IN EXECUTION
Leonardo da Vinci first conceptualized scleral lenses in the early 16th century.1 The first scleral lenses were used to manage ocular surface disease and were actually blown glass scleral shells made with no refractive power.2,3 The brothers Fredrich A. and Albert C. Müller were artificial eye makers with a family business in Wiesbaden, Germany. The scleral lenses designed by the Müller brothers in 1887 were thin, lightweight blown glass lenses with clear corneal regions and white scleral portions.
German ophthalmologist Adolf G.E. Fick described the use of scleral lenses with optics added to correct vision in 1888.4 Fick was interested in keratoconus, and reported on six patients fit with scleral lenses: one with keratoconus and five with corneal opacities.5 He observed clouding of the corneal epithelium (corneal edema), later known as Fick’s phenomenon or Sattler’s veil. He also identified the importance of the scleral lens adaptation process in order for wearers to become more tolerant of lens wear. Fick discovered that inserting scleral lenses with boiled 2% grape sugar solution extended the wearing time for rabbits to 8 to 10 hours before the development of corneal clouding.
In 1889, Eugene Kalt, an ophthalmologist in Paris, described contact lenses used as orthopedic appliances in the treatment of keratoconus6; keratoconus itself had been described by Nottingham in 1854.7 Kalt observed that the lenses changed the shape of the cornea, setting the groundwork that eventually led to orthokeratology and the use of contact lenses as a method for myopia control. Also in 1889, August Müller, a medical student in his final year of formal training, created a scleral lens for himself to correct his own 14 D of high myopia.8
Müller attempted to avoid air bubbles under the lenses by inserting them underwater; this did not improve lens tolerance. He then tried having patients use cocaine eye drops prior to lens insertion, which did not improve corneal toxicity and also enhanced the risk of addiction. The use of physiologic saline solution to insert scleral lenses was described by Henri Dor in the 1890s and remained popular until the early 1940s.9 In 1912, Zeiss produced its first scleral lens diagnostic fitting set for use by ophthalmologists (Figure).1 In 1916, the first diagnostic fitting set designed specifically for keratoconus was produced.10
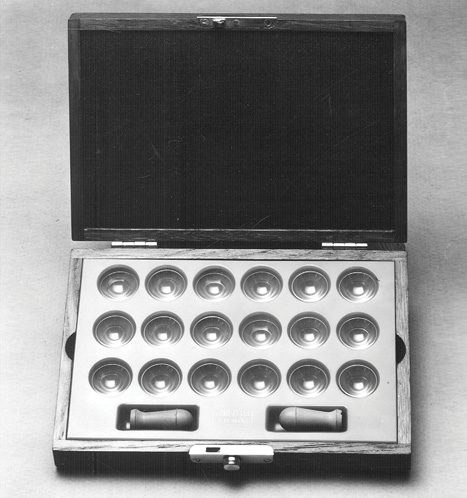
Figure. An early Zeiss scleral lens diagnostic fitting set, circa 1930.

MODERN SCLERAL LENSES
These visionary practitioners had a brilliant concept, but scleral lenses did not work very well at first. Shortcomings included lens-induced corneal edema due to poor transmissibility of oxygen, which eventually led to the discontinuation of lens wear due to corneal hypoxia. In addition, each lens was handmade and impossible to replicate in the event of breakage or loss.
In 1957, Obrig Laboratories produced the Lacrilens, a molded PMMA scleral lens with a large perforation in the lower part of the lens that connected to the central vault by two V-shaped channels.1 In 1967, Fraser and Gordon designed the Apex lens specifically for the UK Hospital Service; its large, semiscleral design provided stable vision, but it was thick and heavy for aphakic prescriptions.11 In many cases, however, the PMMA material led to corneal neovascularization.12 This design is still used, with high-Dk materials, for high prescriptions.
The first rigid gas permeable (RGP) scleral lenses were reported in the 1970s by John James Little and Arthur Irving in the United Kingdom. Despite a lack of a written record of the creation of these lenses, optometric historians consider this to be true.
At the British Contact Lens Association conference in 1983, Australian optometrist Don Ezekiel, Dip Opt (WA), DCLP, reported making scleral lenses using two different RGP materials. These scleral lenses, later manufactured by Gelflex, were approved by the US Food and Drug Administration (FDA) in 2001.
In 1984, Brien Holden, PhD, and George Mertz, OD, reported that the oxygen demand of the cornea was 70 to 75 mm Hg.13 These findings pushed multiple manufacturers to create improved contact lens materials.
In 1985, Rients Visser of Visser Contactlenzen and Visser Contact Lens Practice in Nijmegen, The Netherlands, developed a spherical scleral lens, and production techniques were made possible by Ben Wanders of Procornea. Later improvements in this design, including scleral lenses with back surface toricity, were developed in collaboration between Visser and Wanders.
In 1992, Ken Pullum, BSc, a UK optometrist, founded Innovative Sclerals (since acquired by Bausch + Lomb) in Hertford, United Kingdom, to supply and fit RGP scleral lenses. In his system, an impression was taken of the eye, then the cast was computer-scanned, and the back surface of the lens was lathe cut using CAD/CAM technology. The front surface was finished by hand to keep the overall thickness to an absolute minimum.
In 1994, the nonprofit Boston Foundation for Sight (now BostonSight) gained FDA approval for the Boston Scleral Lens and for lenses now used in prosthetic replacement of the ocular surface ecosystem (PROSE) treatment. In 2013, Christine Sindt, OD, and Keith Parker developed the EyePrintPRO (EyePrint Prosthetics), an impression-based, transparent prosthetic scleral device designed to match the precise contours of the eye. An impression of the eye captures the curvatures of the entire ocular surface with accuracy within 1 µm to 2µm. EyePrintPRO lens options include toric, decentered optics, multifocal, prism, and higher-order aberration correction. In 2017, two scleral lenses—the SynergEyes VS and SynergEyes VS XL (both by SynergEyes)—were released. These bitangential scleral lenses were created via collaboration between Rients Visser, Bart van der Linden, and their respective teams at the Dutch companies Visser Contactlenzen and NKL Contactlenzen. These easy-to-fit scleral lens accommodate a wide variety of patients. The design of the BostonSight Scleral lens, launched in 2017, is based on scleral anatomy. Driven by clinical data, this lens comes in OD and OS anatomic designs, with front surface eccentricity options that improve quantitative and qualitative vision.
With modern advances, scleral lenses have overcome their early limitations and have gained growing popularity around the world. They continue to advance with the pace of modern materials, precise manufacturing, and advanced technology.
- Bowden T. Contact Lenses: The Story. Bower House Publications.
- Turner A. An interrupted story: French translations from Philosophical Transactions in the seventeenth and eighteenth centuries. Notes and Records: The Royal Society Journal of the History of Science. 2008;62(4):341-354.
- Duke-Elder S. Ophthalmic Optics and Refraction. System of Ophthalmology, vol. 5. London: Kimpton;19705:713.
- Fick AE. A contact lens. 1888. (translation). Arch Ophthalmol. 1997;115(1)120-121.
- Pickford JH. On Conical Cornea. Dublin, Ireland: Hodges and Smith; 1844.
- Müller, A. (1889) Brillengläser und hornhautlinsen. Inaugural Dissertation p. 20. University of Kiel.
- Nottingham, J. Practical observations on conical cornea, and on the short sight, and other defects of vision connected with it. London, England: John Churchill;1854.
- Young T. On the mechanism of the eye. Phil Trans R Soc. 1801;16:23-88.
- Dor H. Sur les verres de contact. Arch Ophtalmol Rev Gen Ophtalmol. 1892;11:493-497
- Rugg-Gunn A. Contact Glasses. Br J Ophthalmol. 1931;15(10):549-574.
- Ruben M. The apex lens. Contact Lens. 1967;1(4):14-28.
- Fraser JP, Gordon SP. The ‘Apex’ lens for uniocular aphakia. Ophthal Opt. 1967;7: 1190-1194, 1247-1253.
- Holden GA, Mertz GW. Critical oxygen levels to avoid corneal edema for daily and extended wear contact lenses. Invest Ophthalmol Vis Sci. 1984;25(10): 1161-7.

